Rewiring Balance: Rehabilitation Strategies for Vestibular Dysfunction
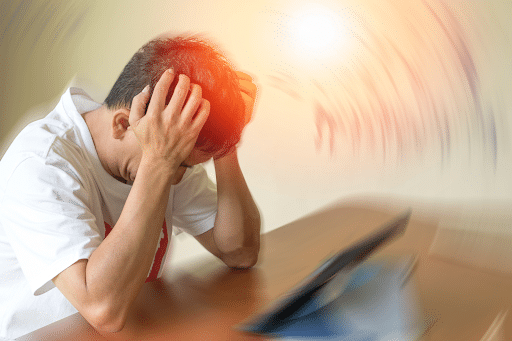
 Vestibular dysfunction can be debilitating, affecting your ability to maintain balance, navigate daily activities, and feel steady in your environment. For many, symptoms such as dizziness, vertigo, and unsteadiness become persistent challenges that interfere with their quality of life. Fortunately, targeted rehabilitation strategies can help restore balance and stability, addressing the root causes of vestibular dysfunction rather than just alleviating the symptoms.
Vestibular dysfunction can be debilitating, affecting your ability to maintain balance, navigate daily activities, and feel steady in your environment. For many, symptoms such as dizziness, vertigo, and unsteadiness become persistent challenges that interfere with their quality of life. Fortunately, targeted rehabilitation strategies can help restore balance and stability, addressing the root causes of vestibular dysfunction rather than just alleviating the symptoms.
At Carolina Brain Center, we focus on holistic and individualized approaches to vestibular rehabilitation. Let’s explore some evidence-based strategies for rewiring balance and reclaiming control over your life.
Understanding Vestibular Dysfunction
The vestibular system, located within the inner ear, is responsible for maintaining balance, spatial orientation, and posture. It works seamlessly with your visual and proprioceptive systems to keep you steady as you move through your environment.
When the vestibular system is impaired due to injury, illness, or other factors, it disrupts these essential functions, leading to symptoms such as:
- Dizziness and vertigo.
- Loss of balance and frequent falls.
- Visual disturbances, such as blurred or jumpy vision.
- Nausea and motion sensitivity.
- Difficulty concentrating or experiencing "brain fog."
Common causes of vestibular dysfunction include benign paroxysmal positional vertigo (BPPV), vestibular neuritis, head trauma, migraines, and age-related degeneration.
Why Rehabilitation with a Functional Neurologist Is Critical
Without targeted rehabilitation, the brain may struggle to adapt to the disrupted signals from the vestibular system. This can lead to compensatory patterns that worsen symptoms over time, such as avoiding movement, over-relying on vision for balance, or developing chronic tension in the neck and shoulders.
Rehabilitation strategies aim to:
- Recalibrate the brain’s ability to process vestibular input.
- Strengthen alternative sensory pathways for balance.
- Reduce dizziness and vertigo.
- Improve overall physical and cognitive function.
By actively engaging the nervous system in retraining exercises, you can rebuild your balance and restore confidence in movement.
Key Rehabilitation Strategies
- Vestibular Rehabilitation Therapy (VRT)
VRT is a specialized form of physical therapy designed to improve balance and reduce dizziness. It uses exercises tailored to the individual’s specific impairments. Components of VRT include:
- Gaze Stabilization: Exercises that train your eyes to stay focused on a target while your head moves, improving visual-vestibular coordination.
- Balance Training: Activities that challenge your ability to maintain stability on various surfaces or during movement.
- Habituation Exercises: Gradual exposure to movements or environments that trigger symptoms, helping the brain adapt and reduce sensitivity.
VRT is evidence-based and widely recognized as one of the most effective treatments for vestibular dysfunction.
- Postural Alignment and Strengthening
A well-aligned posture and strong core muscles are essential for maintaining balance. Weak or imbalanced muscles can exacerbate symptoms by putting undue strain on the vestibular system. Rehabilitation often includes:
- Core strengthening exercises.
- Postural training to improve alignment and reduce neck or back tension.
- Dynamic activities that integrate balance with strength-building movements.
These exercises not only enhance stability but also improve your overall mobility and confidence in daily activities.
- Neurological and Chiropractic Adjustments
At Carolina Brain Center, we recognize the importance of the nervous system’s role in balance. Misalignments in the cervical spine or dysfunctions in neural pathways can contribute to vestibular disorders. Chiropractic adjustments and neurological techniques aim to:
- Restore proper alignment in the spine to reduce tension and improve neural communication.
- Enhance the vestibular system’s ability to coordinate with other sensory systems.
- Support natural healing processes by reducing inflammation and promoting circulation.
- Sensory Integration Therapy
Vestibular dysfunction often creates a sensory mismatch between the inner ear, vision, and proprioception (sense of body position). Sensory integration therapy focuses on improving the coordination between these systems through activities like:
- Balancing on unstable surfaces while focusing on a visual target.
- Eye-tracking exercises combined with body movements.
- Proprioceptive training to enhance spatial awareness and muscle control.
This type of therapy strengthens your brain’s ability to integrate sensory input, reducing symptoms like dizziness and disorientation.
- Lifestyle Modifications for Vestibular Health
Simple changes in your daily routine can support your rehabilitation journey and prevent further disruption to your vestibular system. These include:
- Hydration: Staying properly hydrated to support inner ear function.
- Nutrition: Consuming a balanced diet rich in nutrients that reduce inflammation and support neural health, such as omega-3 fatty acids, antioxidants, and magnesium.
- Stress Management: Chronic stress can exacerbate vestibular symptoms. Techniques like mindfulness, yoga, or deep breathing exercises can help regulate your nervous system.
- Sleep Hygiene: Prioritizing restful sleep allows your brain to heal and recalibrate during rehabilitation.
The Role of Neuroplasticity in Rehabilitation
The success of vestibular rehabilitation lies in the brain’s ability to adapt—a process known as neuroplasticity. Neuroplasticity enables the brain to form new connections and pathways in response to targeted stimulation. Rehabilitation exercises with functional neurology, particularly GyroStim, tap into this natural ability, helping your brain rewire itself to restore balance and reduce symptoms.
A study published in the Journal of Neurologic Physical Therapy highlights the importance of early and consistent rehabilitation in leveraging neuroplasticity to improve outcomes for individuals with vestibular dysfunction.
Why Choose Holistic Rehabilitation at Carolina Brain Center?
At Carolina Brain Center, we believe that effective vestibular rehabilitation requires more than just addressing symptoms. Our approach focuses on understanding the root causes of your dysfunction and tailoring a treatment plan that meets your specific needs. Here’s what sets us apart:
- Personalized Care: We perform comprehensive assessments to identify the precise nature of your vestibular dysfunction and design therapies that align with your goals.
- Holistic Methods: By integrating vestibular therapy, chiropractic care, and lifestyle strategies, we address every aspect of your condition.
- Non-Invasive Solutions: Our focus on drug-free, non-invasive therapies ensures that your recovery supports your overall health. Our utilization of treatment methods such as GyroStim and hyperbaric oxygen therapy (HBOT) in Raleigh positions us at the forefront of the industry.
Regain Your Balance and Confidence
Living with vestibular dysfunction can feel isolating and overwhelming, but rehabilitation offers a path forward. With the right treatment plan, you can retrain your brain, restore your balance, and reclaim your ability to move through life with confidence.
At Carolina Brain Center, we have the expertise and proven results that will help you guide you through the recovery process. Contact us today to schedule a consultation with Dr. Dane. Together, we’ll create a personalized plan to help you regain stability and achieve lasting relief.
The Complex Relationship Between Vestibular Dysfunction and PTSD
 Vestibular dysfunction is often associated with symptoms like dizziness, vertigo, and imbalance. However, its effects can extend far beyond physical symptoms, influencing emotional health and contributing to conditions like post-traumatic stress disorder (PTSD). For individuals living with both vestibular dysfunction and PTSD, the combination can be overwhelming, as one condition often amplifies the other.
Vestibular dysfunction is often associated with symptoms like dizziness, vertigo, and imbalance. However, its effects can extend far beyond physical symptoms, influencing emotional health and contributing to conditions like post-traumatic stress disorder (PTSD). For individuals living with both vestibular dysfunction and PTSD, the combination can be overwhelming, as one condition often amplifies the other.
This article explores the connection between vestibular dysfunction and PTSD, how a brain imbalance contributes to emotional dysregulation, and how a holistic approach—guided by a functional neurologist—can help restore balance and improve quality of life.
Understanding Vestibular Dysfunction and Its Role in Emotional Health
The vestibular system, located in the inner ear, plays a critical role in maintaining balance, spatial orientation, and posture. It sends constant sensory input to the brain about your body’s position relative to gravity and movement. When this system is disrupted, you may experience:
- Dizziness or a spinning sensation (vertigo).
- Difficulty maintaining balance.
- Visual disorientation and spatial confusion.
These symptoms place significant stress on your brain, creating what is often referred to as a brain imbalance—a state where the brain struggles to process conflicting sensory inputs. Over time, this imbalance can lead to heightened anxiety, fear of movement, and emotional dysregulation, creating the perfect storm for developing or worsening PTSD.
The Overlap Between Vestibular Dysfunction and PTSD
PTSD is a mental health condition often triggered by a traumatic event. It is characterized by symptoms like hypervigilance, intrusive thoughts, and heightened emotional reactivity. Surprisingly, vestibular dysfunction and PTSD share significant overlap in both symptoms and brain pathways, including:
- Sensory Processing Disruption
In PTSD, the brain becomes hyperaware of potential threats, leading to exaggerated responses to sensory input. Vestibular dysfunction amplifies this by creating a sensory mismatch between what your body feels and what your eyes perceive, increasing feelings of disorientation and panic. - Autonomic Nervous System Dysregulation
Both conditions disrupt the autonomic nervous system, which regulates critical functions like heart rate, blood pressure, and digestion. You may experience:
- Heart palpitations.
- Sweating or trembling.
- Sudden nausea or dizziness.
This dysregulation creates physical symptoms that mimic anxiety or panic attacks, further exacerbating PTSD.
- Emotional Exhaustion and Hypervigilance
Chronic dizziness or vertigo can trigger a state of hypervigilance, where you constantly monitor your environment for potential triggers. This heightened awareness is a hallmark of PTSD and contributes to feelings of emotional exhaustion, fear, and avoidance behaviors.
Research published in Frontiers in Neurology highlights that individuals with vestibular disorders have a higher likelihood of developing emotional symptoms, including PTSD and generalized anxiety. This connection underscores the importance of addressing vestibular dysfunction as part of a holistic approach to emotional and neurological health.
Symptoms You Shouldn’t Ignore
If you are experiencing both vestibular dysfunction and PTSD, you may notice symptoms like:
- Chronic dizziness, lightheadedness, or vertigo.
- Fear of movement or environments that trigger disorientation.
- Anxiety, hypervigilance, or panic when navigating crowded spaces.
- Difficulty concentrating or experiencing “brain fog.”
- Exaggerated physical responses, like increased heart rate or nausea, in stressful situations.
These symptoms can significantly impact daily life, often leading to social withdrawal, emotional distress, and reduced quality of life. Identifying and addressing both conditions is critical to achieving long-term relief.
How a Functional Neurologist Can Help Restore Balance
At Carolina Brain Center, we take a holistic, drug-free approach to treating vestibular dysfunction and its emotional effects, including PTSD. As a functional neurologist, Dr. Dane specializes in understanding how the vestibular system interacts with the brain and nervous system and developing targeted therapies to address the root cause of your symptoms.
Here’s how we can help:
- Comprehensive Evaluation
We begin with an in-depth evaluation of your vestibular system, nervous system function, and emotional health. By identifying specific imbalances, we can create a treatment plan tailored to your needs. - Vestibular Rehabilitation Therapy (VRT)
VRT involves carefully designed exercises that retrain your brain to process sensory inputs more effectively. This therapy helps reduce dizziness, improve balance, and decrease the sensory conflicts that trigger emotional responses. - Neurological Adjustments
Gentle, targeted adjustments to your spine and nervous system can restore communication between the brain and vestibular system. This approach addresses the brain imbalance contributing to your symptoms, promoting better nervous system regulation and reducing hypervigilance. - Integration of Mind-Body Techniques
Addressing the connection between your brain and body is critical to breaking the cycle of vestibular dysfunction and PTSD. We incorporate:
- Balance and grounding exercises to reduce anxiety in disorienting situations.
- Breathing techniques to calm your autonomic nervous system.
- Stress management strategies that support emotional regulation and recovery.
- Lifestyle Recommendations
Simple, holistic changes—like improving sleep quality, proper hydration, and mindful movement—can support vestibular and emotional health. These foundational adjustments promote long-term recovery and resilience.
Why Early Intervention Matters
When vestibular dysfunction and PTSD coexist, untreated symptoms can perpetuate each other, creating a cycle of physical and emotional distress. Early intervention is key to restoring your body’s ability to function properly and improving your quality of life.
A functional neurologist’s holistic approach addresses the brain imbalance and autonomic dysregulation that underpin both conditions, helping you achieve lasting relief.
Regain Control and Find Relief
Living with vestibular dysfunction and PTSD can be overwhelming, but you don’t have to face it alone. At Carolina Brain Center, we specialize in identifying and treating the underlying causes of your symptoms. By addressing the root of the problem with holistic, evidence-based care, we help you restore balance—both physically and emotionally.
If you’re struggling with dizziness, emotional dysregulation, or symptoms of PTSD, contact us today to schedule a consultation with Dr. Dane. As an expert in vestibular health and neurological care, she is here to guide you toward recovery with compassion and expertise.
Motion Sickness and Vertigo: The Holistic Path to Relief
 Motion sickness and vertigo are debilitating conditions that affect your ability to navigate daily life with ease. While they share overlapping symptoms—like dizziness, nausea, and disorientation—their causes and treatments can differ. Regardless of the cause, finding effective, holistic solutions is essential to regaining your quality of life.
Motion sickness and vertigo are debilitating conditions that affect your ability to navigate daily life with ease. While they share overlapping symptoms—like dizziness, nausea, and disorientation—their causes and treatments can differ. Regardless of the cause, finding effective, holistic solutions is essential to regaining your quality of life.
At Carolina Brain Center, we specialize in addressing these conditions using natural, prescription drug-free methods tailored to your unique needs. If you’re searching for doctors who treat motion sickness or doctors who treat vertigo, understanding the underlying causes and holistic options can guide you toward lasting relief.
What Causes Motion Sickness and Vertigo?
Motion sickness occurs when your brain receives conflicting signals from your sensory systems. For example, when you’re reading a book in a moving car, your inner ear senses motion, but your eyes don’t detect it. This sensory mismatch can lead to nausea, dizziness, and discomfort.
Vertigo, on the other hand, is typically caused by an issue within the vestibular system, which controls your sense of balance and spatial orientation. Common causes include:
- Inner Ear Disorders: Conditions like benign paroxysmal positional vertigo (BPPV) or vestibular neuritis.
- Head Injuries: Concussions or trauma can disrupt the vestibular pathways.
- Vestibular Migraine: A neurological condition that combines migraine symptoms with dizziness.
For both conditions, the symptoms can interfere with daily activities, making it essential to seek medical help when you begin to experience them.
Signs You May Need Vertigo Treatment
If you’re experiencing symptoms like dizziness, spinning sensations, nausea, or difficulty maintaining balance, you may benefit from vertigo treatment in Raleigh. Common signs include:
- A sense of the world spinning or moving when you’re stationary.
- Difficulty walking or standing upright.
- Feeling unsteady in environments with moving objects, like escalators or crowded spaces.
- Persistent nausea, especially during specific activities or movements.
These symptoms not only disrupt physical comfort but can also lead to emotional challenges and avoidance behaviors.
How Holistic Care Can Address Motion Sickness and Vertigo
At Carolina Brain Center, our approach to motion sickness and vertigo is rooted in addressing the underlying causes rather than focusing solely on symptom management. By integrating advanced diagnostic techniques and natural therapies, we aim to create a comprehensive plan tailored to each individual. Here’s how we provide care that stands out:
- Precision Diagnosis
Effective care begins with a thorough understanding of your condition. Using advanced diagnostic tools, we assess the functionality of your vestibular system, postural stability, and nervous system integration. This allows us to pinpoint the specific factors contributing to your motion sickness or vertigo, whether they involve vestibular dysfunction, sensory mismatches, or neural miscommunication. - Vestibular System Optimization
The vestibular system is central to balance and spatial awareness. Dysfunction in this system is often at the root of vertigo and motion sickness. At our center, we employ therapies specifically designed to recalibrate and enhance vestibular function. These include:
- Targeted balance training to improve coordination and stability.
- Sensory integration exercises that encourage your brain to adapt to and reconcile conflicting inputs from the eyes, inner ear, and body.
By retraining your brain to process movement-related signals more effectively, we address the core issues causing dizziness and discomfort.
- Neurological and Structural Alignment
A properly functioning nervous system is key to resolving motion sickness and vertigo. Misalignments in the spine or tension in the neck can exacerbate vestibular symptoms by disrupting the communication between your brain and body. As chiropractic neurologists, we use gentle, precise adjustments to restore this connection, allowing your nervous system to function optimally. This often leads to significant improvements in balance, orientation, and overall well-being. - Enhancing Postural Stability and Muscle Engagement
Postural control is an essential aspect of balance. Weak core muscles or imbalances in posture can increase the severity of vertigo and motion sickness. We guide patients through personalized programs designed to:
- Strengthen key muscle groups that support postural control.
- Improve awareness of body alignment during movement and stillness.
This comprehensive approach helps you achieve a more stable foundation for navigating daily activities.
- Emphasizing Holistic Wellness
In addition to physical therapies, we consider lifestyle factors that may contribute to your symptoms. For example:
- Stress Reduction: Chronic stress can intensify vestibular symptoms. Incorporating relaxation techniques such as mindfulness, yoga, or breathing exercises into your daily routine can help calm the nervous system.
- Nutritional Support: Proper hydration and a balanced diet rich in nutrients that support neural health, like omega-3 fatty acids and antioxidants, play a vital role in maintaining vestibular function.
By addressing these foundational aspects of wellness, we ensure your care plan supports not only your vestibular health but also your overall quality of life.
Why Choose Holistic Treatment?
Holistic care focuses on treating the person, not just the condition. At Carolina Brain Center, we believe that lasting relief from motion sickness and vertigo comes from addressing the body as a whole.
If you’re looking for vertigo treatment in Raleigh, here’s what sets us apart:
- Personalized Care: Every individual experiences motion sickness and vertigo differently. We tailor your treatment plan to meet your unique needs.
- Drug-Free Solutions: We focus on natural therapies to promote healing without relying on medications.
- Expertise in Vestibular Health: As doctors who treat motion sickness and vertigo, we specialize in advanced diagnostic and therapeutic techniques designed to restore balance and harmony to your body.
Take the First Step Toward Balance and Comfort
Living with motion sickness or vertigo doesn’t have to limit your life. Whether you’re dealing with dizziness in cars, difficulty navigating crowded spaces, or persistent spinning sensations, the right care can help you regain your confidence and stability.
At Carolina Brain Center, Dr. Dane is dedicated to providing effective, holistic care for motion sickness and vertigo. If you’re searching for long lasting relief for the debilitating conditions associated with vertigo and motion sickness, contact us today to schedule a consultation. Together, we will develop a personalized plan to help you find lasting relief and get back to enjoying the activities you love.
Understanding How Vestibular Dysfunction Impacts Cognitive and Emotional Health
 The brain is a marvel of interconnected systems, working in harmony to regulate your thoughts, emotions, and physical balance. When one of these systems, such as the vestibular system, is disrupted, the effects can cascade into areas you might not expect—like cognition and emotional well-being. Vestibular dysfunction, while often associated with physical symptoms like dizziness or imbalance, can also lead to cognitive difficulties and emotional challenges, including anxiety, depression, and even post-traumatic stress disorder (PTSD).
The brain is a marvel of interconnected systems, working in harmony to regulate your thoughts, emotions, and physical balance. When one of these systems, such as the vestibular system, is disrupted, the effects can cascade into areas you might not expect—like cognition and emotional well-being. Vestibular dysfunction, while often associated with physical symptoms like dizziness or imbalance, can also lead to cognitive difficulties and emotional challenges, including anxiety, depression, and even post-traumatic stress disorder (PTSD).
Let’s explore how vestibular dysfunction contributes to cognitive and emotional imbalances, the role of chemical changes in the brain, and how a functional neurologist can help restore harmony and improve your quality of life.
The Vestibular System and Its Role in Brain Function
Your vestibular system, housed within the inner ear, is responsible for detecting motion and maintaining balance. However, its influence extends far beyond physical stability. It directly communicates with the brain’s limbic system (which regulates emotions) and cortical areas involved in spatial awareness and memory.
When the vestibular system malfunctions, the resulting sensory mismatch can create a ripple effect in the brain, leading to what some refer to as a brain imbalance. This imbalance not only affects your ability to maintain physical stability but also disrupts your emotional and cognitive functions.
Cognitive Effects of Vestibular Dysfunction
- Brain Fog and Memory Issues
One of the most common cognitive symptoms of vestibular dysfunction is brain fog—a feeling of mental sluggishness or confusion. You might find it harder to concentrate, retain information, or stay organized. This cognitive strain arises from the brain’s effort to compensate for conflicting signals from the vestibular system. - Impaired Spatial Awareness
The vestibular system plays a key role in helping you understand your position in space. When it’s not functioning properly, tasks like driving, navigating new environments, or even walking can feel disorienting. - Fatigue and Reduced Mental Clarity
Vestibular dysfunction increases the cognitive load on your brain as it works overtime to process sensory inputs. This heightened effort often leads to fatigue and reduced clarity in decision-making.
Emotional Consequences of Vestibular Dysfunction
The connection between vestibular dysfunction and emotional health is deeply rooted in the brain’s chemistry. A chemical imbalance in the brain often accompanies vestibular dysfunction, affecting the regulation of neurotransmitters like serotonin and dopamine. These imbalances can result in:
- Anxiety and Panic Attacks
Vestibular dysfunction frequently triggers anxiety due to the brain’s heightened sensitivity to disorienting sensations like dizziness or vertigo. Panic attacks can occur as the body reacts to these unfamiliar and uncomfortable sensations. - Depression
Chronic dizziness and balance issues can lead to feelings of helplessness and social withdrawal, increasing the risk of depression. The chemical imbalance in the brain caused by disrupted vestibular inputs exacerbates this emotional toll. - PTSD and Vestibular Dysfunction
In some cases, vestibular dysfunction can contribute to or worsen post-traumatic stress disorder (PTSD). The brain’s limbic system, already sensitized by trauma, may become further dysregulated by vestibular imbalances, intensifying emotional responses.
What Causes Brain and Emotional Imbalances in Vestibular Dysfunction?
Vestibular dysfunction can arise from a variety of conditions, including:
- Inner Ear Disorders: Conditions like Ménière’s disease or vestibular neuritis disrupt the brain’s ability to process balance-related signals.
- Head Injuries: Concussions or other traumas can damage the pathways connecting the vestibular system to the brain, leading to a brain imbalance.
- Chronic Stress: Prolonged stress can amplify vestibular symptoms and disrupt the body’s ability to regulate neurotransmitters, resulting in a chemical imbalance in the brain.
According to a study published in Frontiers in Neurology, the interaction between vestibular dysfunction and the limbic system highlights the critical role of the vestibular system in maintaining both cognitive and emotional balance.
How a Functional Neurologist Can Help
If you’re struggling with the effects of vestibular dysfunction, a chiropractic neurologist can provide a holistic, non-invasive approach to treatment. At Carolina Brain Center, we specialize in addressing the root causes of brain imbalances and restoring harmony to your nervous system.
Here’s how we can help:
- Comprehensive Evaluation
We use advanced diagnostic tools to assess your vestibular system, cognitive function, and emotional health. This thorough evaluation allows us to pinpoint the source of your brain imbalance and develop a personalized treatment plan. - Targeted Vestibular Rehabilitation
Vestibular rehabilitation therapy (VRT) is designed to recalibrate the brain’s response to balance-related signals. This therapy not only improves physical stability but also alleviates cognitive and emotional symptoms by addressing the underlying chemical imbalances in the brain. - Neurological Adjustments
Gentle, targeted adjustments to the spine and nervous system can enhance communication between the vestibular system and the brain. These adjustments promote better balance, reduce dizziness, and support emotional stability. - Lifestyle Modifications
Simple changes, such as improving hydration, sleep habits, and stress management, can support your brain’s natural ability to heal and rebalance itself. - Emotional Support
Addressing the emotional toll of vestibular dysfunction is just as important as treating the physical symptoms. We integrate cognitive-behavioral techniques and relaxation strategies into your care plan to help you regain confidence and peace of mind.
Breaking the Cycle of Brain Imbalance
Living with vestibular dysfunction can feel like an unending cycle of physical and emotional challenges. The disorientation caused by brain imbalances feeds into anxiety, which in turn worsens vestibular symptoms. This cycle can be frustrating and overwhelming, but it’s not permanent.
By addressing the root causes of vestibular dysfunction, including any associated chemical imbalances in the brain, you can regain control of your cognitive and emotional health.
Take the Next Step Toward Healing
The connection between vestibular dysfunction, cognition, and emotions underscores the importance of a comprehensive approach to treatment. At Carolina Brain Center, we are committed to helping you find relief through targeted therapies, personalized care, and a deep understanding of the brain’s complexities.
If you’re experiencing symptoms of dizziness, cognitive difficulties, or emotional distress, don’t wait to seek help. Contact us today to schedule a consultation with Dr Dane, the top functional neurologist in Raleigh, who can guide you on your journey to recovery. Together, we’ll help you restore balance to your brain and reclaim your quality of life.
Vestibular Dysfunction and Anxiety: Unveiling the Hidden Connection
 Vestibular dysfunction is a complex condition that affects balance, spatial orientation, and stability. However, its impact extends beyond physical symptoms, influencing emotional and psychological health, particularly in the form of heightened anxiety. The intricate relationship between vestibular dysfunction and anxiety is not fully understood but involves a multifaceted interplay of neurophysiological mechanisms, sensory processing, and emotional regulation.
Vestibular dysfunction is a complex condition that affects balance, spatial orientation, and stability. However, its impact extends beyond physical symptoms, influencing emotional and psychological health, particularly in the form of heightened anxiety. The intricate relationship between vestibular dysfunction and anxiety is not fully understood but involves a multifaceted interplay of neurophysiological mechanisms, sensory processing, and emotional regulation.
This article delves into the connection between vestibular dysfunction and anxiety, examining how the vestibular system interacts with the brain and autonomic nervous system, the clinical manifestations of this relationship, and evidence-based approaches to treatment.
The Role of the Vestibular System in Anxiety
The vestibular system, housed within the inner ear, plays a vital role in maintaining balance and spatial awareness. It sends signals to various brain regions, including the cerebellum, brainstem, and cortical areas, to help orient the body in space. Beyond its motor functions, the vestibular system also interacts with the limbic system, which regulates emotions, including fear and anxiety.
When the vestibular system malfunctions, it disrupts the brain’s ability to integrate sensory inputs from vision, proprioception, and vestibular signals. This sensory mismatch can trigger feelings of disorientation, dizziness, and imbalance, which are commonly associated with anxiety. Furthermore, chronic vestibular dysfunction can lead to hypervigilance, avoidance behaviors, and a heightened state of arousal, further perpetuating anxiety.
Clinical Manifestations of Vestibular-Induced Anxiety
Patients with vestibular disorders often report overlapping physical and psychological symptoms, including:
- Persistent Dizziness: A subjective sensation of spinning or imbalance, even when stationary.
- Vertigo: An intense spinning sensation that can induce panic and fear.
- Heightened Sensitivity to Movement: Exaggerated responses to visual or physical motion.
- Hypervigilance: A constant state of alertness, driven by the fear of triggering dizziness or falling.
- Avoidance Behaviors: Patients may limit activities like driving, climbing stairs, or navigating crowded spaces to avoid provoking symptoms.
A study published in Frontiers in Neurology found that patients with vestibular disorders had significantly higher levels of anxiety and depression compared to the general population. This correlation underscores the profound psychological burden associated with vestibular dysfunction.
Neurophysiological Mechanisms Linking Vestibular Dysfunction and Anxiety
- Vestibulo-Limbic Connection
The vestibular system directly communicates with the limbic system, including the amygdala and hippocampus, which are central to processing fear and memory. Dysregulation in this pathway can amplify emotional responses to balance-related sensations, contributing to anxiety and panic. - Autonomic Nervous System Dysregulation
Vestibular dysfunction often disrupts the vestibulo-autonomic reflex, leading to abnormal regulation of the autonomic nervous system. This can manifest as:- Increased heart rate (tachycardia).
- Elevated blood pressure.
- Sweating and gastrointestinal disturbances.
These autonomic symptoms are hallmark features of anxiety and further blur the distinction between vestibular and psychological disorders.
- Cognitive Load and Sensory Mismatch
The brain’s attempt to reconcile conflicting sensory inputs places an increased cognitive load on the patient. This heightened demand can lead to fatigue, difficulty concentrating, and emotional exhaustion, exacerbating anxiety.
Differentiating Vestibular Dysfunction from Primary Anxiety Disorders
While anxiety is a common response to vestibular dysfunction, distinguishing it from primary anxiety disorders is critical for appropriate treatment. Key differentiators include:
- Symptom Trigger: Anxiety secondary to vestibular dysfunction often coincides with dizziness or balance disturbances, while primary anxiety disorders may occur independently.
- Pattern of Avoidance: Vestibular-related anxiety typically involves avoidance of activities that provoke physical symptoms, such as motion or crowded environments.
- Response to Vestibular Therapy: Patients with vestibular-induced anxiety often experience symptom relief with vestibular rehabilitation, suggesting a direct link to underlying vestibular dysfunction.
A comprehensive evaluation, including vestibular testing and psychological assessment, is essential for accurate diagnosis.
Treatment Approaches for Vestibular Dysfunction and Anxiety
Management of vestibular dysfunction with coexisting anxiety requires an integrative approach that addresses both the physical and psychological aspects of the condition.
- Vestibular Rehabilitation Therapy (VRT)
VRT is a cornerstone treatment for vestibular dysfunction. It involves a series of exercises designed to improve balance, reduce dizziness, and recalibrate the brain’s response to vestibular signals. By gradually exposing patients to balance challenges, VRT can also desensitize the fear and anxiety associated with movement. - Chiropractic Neurology Interventions
At Carolina Brain Center, we use targeted chiropractic neurology techniques to optimize the nervous system's function. Gentle spinal adjustments, cranial therapies, and vestibular exercises (VRT) can enhance communication between the vestibular system and the brain, promoting better balance and reducing anxiety-inducing symptoms. - Lifestyle Modifications
Simple changes, such as staying hydrated, improving sleep hygiene, and engaging in regular physical activity, can support vestibular and emotional health. Stress management techniques like mindfulness and meditation can also alleviate symptoms.
The Importance of Early Intervention
Delays in addressing vestibular dysfunction can lead to chronic anxiety and a diminished quality of life. Early intervention not only alleviates physical symptoms but also prevents the psychological sequelae that often accompany vestibular disorders.
According to the Vestibular Disorders Association (VeDA), patients who receive timely and multidisciplinary care for vestibular dysfunction are more likely to achieve long-term symptom relief and regain their quality of life.
How Carolina Brain Center Can Help
The connection between vestibular dysfunction and anxiety highlights the intricate relationship between physical and emotional health. By addressing both the vestibular and psychological components of this condition, patients can achieve significant improvements in their symptoms and overall well-being.
At Carolina Brain Center, we specialize in comprehensive, patient-centered care for vestibular dysfunction and related anxiety. With advanced diagnostics, targeted therapies, and a holistic, non-invasive approach, we strive to help you regain balance, stability, and peace of mind.
If you’re experiencing symptoms of dizziness, vertigo, or anxiety, contact us today to schedule a consultation with Dr. Dane. Together, we can develop a personalized treatment plan to restore your health and well-being.
The Vestibulo-Autonomic Reflex (VAR): How Your Inner Ear Affects Your Autonomic System
 Your vestibular system isn’t just about balance—it also plays a surprising role in regulating your autonomic functions, such as heart rate, blood pressure, and even digestion. This connection is managed by the vestibulo-autonomic reflex (VAR), which links your inner ear to your body’s autonomic nervous system.
Your vestibular system isn’t just about balance—it also plays a surprising role in regulating your autonomic functions, such as heart rate, blood pressure, and even digestion. This connection is managed by the vestibulo-autonomic reflex (VAR), which links your inner ear to your body’s autonomic nervous system.
When your head moves or your body changes position, the VAR ensures that your heart rate and blood pressure adjust accordingly. For example, when you stand up quickly, this reflex prevents you from feeling light-headed or faint by stabilizing blood flow to your brain.
However, when the VAR isn’t functioning correctly, you may experience symptoms like vertigo and dizziness, heart palpitations, or even nausea. These symptoms can disrupt your daily life, leaving you searching for relief.
At Carolina Brain Center, we understand how issues with the vestibulo-autonomic reflex can affect your overall well-being. As a chiropractic neurologist, Dr Dane brings 20 years of experience to the practice, and specializes in diagnosing and treating these dysfunctions to help you regain control of your health.
How Does the Vestibulo-Autonomic Reflex Work?
The VAR operates as a communication bridge between your vestibular system and your autonomic nervous system. When your inner ear detects movement or changes in position, it sends signals to your brainstem. The brainstem then coordinates adjustments in your heart rate, blood pressure, and other autonomic functions to maintain your body’s equilibrium.
One key aspect of this reflex is the vestibulo-sympathetic reflex, which activates the sympathetic nervous system during motion. For example:
- Heart rate adjustments: Ensuring your heart pumps faster during physical activity.
- Blood pressure regulation: Preventing a drop in blood pressure when you stand up quickly.
- Sweating: Triggering perspiration to cool your body during exertion.
Signs and Symptoms of VAR Dysfunction
When the vestibulo-autonomic reflex isn’t working properly, you may notice a range of symptoms, such as:
- Dizziness and vertigo: Feeling light-headed or experiencing a spinning sensation.
- Heart palpitations: Unexplained rapid or irregular heartbeats.
- Nausea: Especially during activities like riding in a car or standing up suddenly.
- Orthostatic hypotension: Feeling faint or dizzy when transitioning from sitting to standing.
- Motion sickness: Sensitivity to movement, even during mild activities like walking or riding an elevator.
These symptoms often overlap with other vestibular dysfunctions, making an accurate diagnosis crucial.
Common Causes of VAR Dysfunction
Several factors can disrupt the vestibulo-autonomic reflex, including:
- Vestibular Disorders: Conditions like vestibular neuritis or Ménière's disease can interfere with the inner ear’s ability to communicate with the autonomic nervous system.
- Concussions and Head Injuries: Trauma can damage the pathways that connect your vestibular and autonomic systems.
- Chronic Stress: Persistent stress can overstimulate the autonomic nervous system, worsening vestibular symptoms.
- Postural Issues: Poor posture or spinal misalignments can disrupt the flow of signals between your vestibular system and brainstem.How a Chiropractic Neurologist Can Help
At Carolina Brain Center, we take a holistic approach to addressing vestibulo-autonomic dysfunction. We focus on treating the root causes of your symptoms rather than just masking them.
Here’s how we can help:
- Comprehensive Evaluation: We use advanced testing to assess your vestibular system and autonomic function, pinpointing the exact source of your symptoms.
- Targeted Rehabilitation: Exercises designed to recalibrate your vestibular and autonomic systems can help improve your body’s responses to motion and position changes.
- Neurological Adjustments: Gentle adjustments to your spine and neck can enhance communication between your vestibular system and brainstem, promoting proper autonomic function.
- Lifestyle Modifications: Recommendations for hydration, nutrition, and stress management can support your overall recovery.
By addressing your vestibulo-autonomic dysfunction, we aim to not only alleviate your symptoms but also improve your overall quality of life.
Backed by Science: The Link Between Vestibular and Autonomic Systems
Research has confirmed the strong connection between vestibular function and autonomic regulation. A study published in the Frontiers in Neurology highlights how vestibular dysfunction can lead to significant autonomic disturbances, including dizziness, orthostatic intolerance, and motion sensitivity. The study emphasizes the importance of targeted therapies in addressing these interconnected systems.
Take Control of Your Symptoms
Living with symptoms like dizziness, vertigo, or heart palpitations can feel overwhelming, but understanding the role of your vestibulo-autonomic reflex is the first step toward relief. At Carolina Brain Center, we specialize in identifying and treating these complex dysfunctions through a personalized, non-invasive approach.
If you’re ready to take control of your symptoms and improve your quality of life, contact us today to schedule a consultation with Dr. Dane. We are committed to helping you restore the balance and stability essential to your well-being.
Balancing Acts: The Vestibulo-Spinal Reflex (VSR) and Postural Control
 The vestibulo-spinal reflex (VSR) is a crucial system in your body that helps maintain balance and posture. Anytime you walk, run, or even stand still, your VSR is hard at work, ensuring your body stays stable and upright. It does this by coordinating information from your inner ear, muscles, and nervous system to make continuous adjustments to your posture.
The vestibulo-spinal reflex (VSR) is a crucial system in your body that helps maintain balance and posture. Anytime you walk, run, or even stand still, your VSR is hard at work, ensuring your body stays stable and upright. It does this by coordinating information from your inner ear, muscles, and nervous system to make continuous adjustments to your posture.
When your VSR is functioning properly, you barely notice it. But when something goes wrong—like after an injury, illness, or chronic stress—you may experience symptoms such as dizziness, vertigo, or even frequent falls.
At Carolina Brain Center, we understand how these symptoms can disrupt your life. As a chiropractic neurologist in Raleigh, NC, Dr Dane specializes in helping patients with dizziness and vertigo regain their balance and improve their quality of life.
How Does the Vestibulo-Spinal Reflex Work?
The VSR relies on signals from your vestibular system, which is housed in your inner ear. This system detects changes in head position and sends signals to your muscles to adjust your posture.
Here are two key components of the VSR:
- Vestibulo-Colic Reflex: This reflex stabilizes your head during movement, preventing it from bobbing or wobbling when you walk or turn.
- Cervico-Colic Reflex: This reflex works in tandem with the vestibulo-colic reflex to maintain proper alignment of your head and neck, ensuring smooth, coordinated movements.
Together, these reflexes form the foundation of your balance system, allowing you to move with confidence and stability.
Signs and Symptoms of VSR Dysfunction
When your VSR isn’t working properly, you may experience symptoms such as:
- Dizziness and vertigo: A spinning sensation or feeling off-balance.
- Frequent falls: Difficulty maintaining your footing, especially on uneven surfaces.
- Poor posture: Slouching or difficulty standing upright without discomfort.
- Neck stiffness or pain: As your body compensates for instability, tension can build in your neck and shoulders.
These symptoms can range from mild to severe, but they all indicate that your body’s balance system needs attention.
Common Causes of VSR Dysfunction
Several factors can disrupt the vestibulo-spinal reflex, including:
- Vestibular Disorders: Conditions like vestibular neuritis or labyrinthitis can interfere with the signals your inner ear sends to your muscles.
- Concussions and Head Injuries: Trauma can damage the pathways that connect your vestibular system to your spine and muscles.
- Aging: Natural wear and tear on your vestibular system and muscles can lead to decreased balance and stability.
- Chronic Stress: Prolonged stress can heighten muscle tension and exacerbate symptoms of dizziness and vertigo.
According to the Vestibular Disorders Association (VeDA), balance disorders affect millions of people each year, often leading to significant disruptions in daily activities.
How a Chiropractic Neurologist Can Help
If you’re dealing with dizziness, vertigo, or balance issues, seeing a chiropractic neurologist could be the solution you’ve been looking for. At Carolina Brain Center, we take a holistic and personalized approach to treating vestibular and postural dysfunctions.
Here’s how we can help:
- Detailed Evaluation: We use advanced diagnostic tools to assess your vestibulo-spinal reflex, balance, and overall posture.
- Targeted Rehabilitation: Customized exercises can retrain your body to respond correctly to balance challenges. This might include postural training or dynamic stability exercises.
- Neurological Adjustments: Gentle spinal and cervical adjustments can improve the communication between your vestibular system and the rest of your body.
- Lifestyle Recommendations: Small changes in your daily habits—like staying hydrated or practicing stress management—can make a big difference in your recovery.
Our goal is to address the root cause of your symptoms and empower you to move confidently again.
Why Early Treatment Is Important
Ignoring symptoms of VSR dysfunction can lead to further complications, including:
- Increased risk of injury from falls.
- Chronic neck and back pain due to poor posture.
- Anxiety or fear of movement caused by instability.
By seeking treatment early, you can prevent these issues and restore your balance and confidence.
Backed by Science: The Importance of Vestibular Rehabilitation
Research shows that vestibular rehabilitation can significantly improve balance and reduce symptoms of dizziness and vertigo. According to a study published in the Journal of Physical Therapy Science, targeted exercises and therapy can help patients regain stability and improve their quality of life.
At Carolina Brain Center, we incorporate both evidence-based practices as well as Dr. Dane’s proprietary techniques into our treatment plans to provide you with the best possible outcomes.
Take the First Step Toward Balance and Stability
Living with dizziness and vertigo can feel overwhelming, but you don’t have to navigate it alone. The vestibulo-spinal reflex is essential for your balance, and when it’s not working as it should, it’s time to seek help.
At Carolina Brain Center, we specialize in helping patients like you regain their balance and improve their quality of life. Through a combination of advanced diagnostics, personalized treatment, and holistic care, we can help you find relief and get back to doing the things you love.
Ready to take the first step? Contact us today to schedule your evaluation and learn more about how a chiropractic neurologist can help you.
Understanding the Vestibulo-Ocular Reflex (VOR): Keeping Your Vision Stable During Movement
 The vestibulo-ocular reflex (VOR) is one of the most crucial systems in your body for maintaining stable vision during head movements. Whether you’re walking, running, or simply turning your head, the VOR ensures that your eyes remain focused on a target, so your surroundings don’t appear blurry or disorienting.
The vestibulo-ocular reflex (VOR) is one of the most crucial systems in your body for maintaining stable vision during head movements. Whether you’re walking, running, or simply turning your head, the VOR ensures that your eyes remain focused on a target, so your surroundings don’t appear blurry or disorienting.
Your inner ear and eyes work together to achieve this stability. The VOR detects your head’s motion and adjusts your eye movements to compensate, keeping your vision clear. When this system isn’t functioning properly, you may experience dizziness, blurred vision, or even nausea—symptoms that can disrupt your daily life and leave you searching for answers.
At Carolina Brain Center, we specialize in identifying and treating VOR dysfunction. By understanding this reflex and how it affects you, we can develop effective, personalized treatment plans that help you regain control of your balance and clarity.
How Does the Vestibulo-Ocular Reflex Work?
The VOR is powered by your vestibular system, a sophisticated network located in your inner ear. This system detects movement and sends signals to your brainstem, which then instructs your eyes to move in the opposite direction of your head. This coordination allows you to maintain focus on a fixed point, no matter how your head moves.
The VOR has three main components:
- Canal-Ocular Reflex: This part handles angular movements, like when you shake your head “no.”
- Otolith-Ocular Reflex: This component processes linear movements, such as moving forward or backward or when you encounter changes in gravity.
- Ocular-Tilt Reflex (OTR): This reflex adjusts your eye alignment to maintain proper orientation when you tilt your head.
Each of these functions is critical for maintaining stable vision and balance during everyday activities.
Signs and Symptoms of VOR Dysfunction
When your VOR isn’t functioning correctly, you may notice symptoms like:
- Dizziness or vertigo: A sensation that you or your surroundings are spinning.
- Blurred or unstable vision: Difficulty focusing, especially during movement.
- Nausea or motion sickness: Feeling queasy while riding in a car, boat, or plane.
- Balance problems: Struggling to stay steady on your feet, particularly in busy or uneven environments.
These symptoms can stem from various underlying causes, such as injury, illness, or even chronic stress.
Common Causes of VOR Dysfunction
Several conditions can affect your VOR, including:
- Vestibular Disorders: Inner ear problems like vestibular neuritis or Ménière's disease can disrupt the signals needed for proper eye movement.
- Concussions and Head Injuries: Trauma can impair the neural pathways connecting your vestibular system and eyes, leading to ongoing symptoms.
- Aging: As you age, natural degeneration in the vestibular system may lead to dizziness or balance problems.
- Stress and Anxiety: Chronic stress can amplify vestibular symptoms, creating a cycle of discomfort and tension.
According to the National Institute on Deafness and Other Communication Disorders (NIDCD), vestibular disorders are a common cause of dizziness and balance issues, affecting millions of people annually. Recognizing these conditions early can lead to more effective treatment.
How Carolina Brain Center Can Help You
If you’re dealing with symptoms of VOR dysfunction, Carolina Brain Center offers a unique approach to treatment. As chiropractic neurologists, we specialize in holistic healthcare, an approach that is non-invasive, drug-free, and tailored to your specific needs.
Here’s how we can help:
- Comprehensive Evaluation: We use advanced diagnostic techniques to assess your vestibular function, including balance tests and eye movement analysis.
- Vestibular Rehabilitation: Through targeted exercises, we help retrain your VOR to respond correctly to movement. For example, gaze stabilization exercises can improve your ability to focus while moving your head.
- Neurological Adjustments: Gentle, precise adjustments to your spine and neck can improve the communication between your vestibular system and your brain.
- Lifestyle Guidance: Simple changes in hydration, nutrition, and stress management can support your recovery and improve your overall quality of life.
At Carolina Brain Center, we’re committed to helping you find relief and restore balance—both physically and emotionally.
Why Early Intervention Matters
Ignoring symptoms of VOR dysfunction can lead to more serious problems, such as:
- Increased risk of falls or accidents.
- Reduced independence due to fear of movement.
- Heightened anxiety and emotional stress.
By seeking treatment early, you can prevent these complications and get back to living the life you enjoy.
Scientific Backing for VOR Treatments
Research supports the effectiveness of vestibular rehabilitation in treating VOR dysfunction. According to a study published in the Journal of Neurology, vestibular exercises can significantly reduce dizziness and improve balance in patients with vestibular disorders. These findings highlight the importance of targeted therapies like those offered at Carolina Brain Center.
Prioritizing Your Vestibular Health
Your vestibulo-ocular reflex plays a vital role in helping you navigate the world with clarity and confidence. When this system isn’t working properly, the effects can be overwhelming—but they’re treatable.
At Carolina Brain Center, we focus on addressing the root causes of your symptoms to provide lasting relief. If you’re tired of dealing with dizziness, blurred vision, or balance issues, let us help you take the first step toward recovery. Contact us today to schedule an evaluation and learn more about how our expertise can benefit you.
The Blood-Brain Barrier and Its Role in Concussion Recovery
 The brain is a highly sensitive organ that requires a protective barrier to shield it from harmful substances in the bloodstream. This barrier, known as the blood-brain barrier (BBB), is essential for maintaining the brain's stable environment and preventing the entry of pathogens, toxins, and other damaging agents. However, when a concussion occurs, the integrity of the BBB can be compromised. This disruption can lead to a multitude of problems that affect both the immediate and long-term recovery process, potentially contributing to conditions such as Post-Concussion Syndrome (PCS).
The brain is a highly sensitive organ that requires a protective barrier to shield it from harmful substances in the bloodstream. This barrier, known as the blood-brain barrier (BBB), is essential for maintaining the brain's stable environment and preventing the entry of pathogens, toxins, and other damaging agents. However, when a concussion occurs, the integrity of the BBB can be compromised. This disruption can lead to a multitude of problems that affect both the immediate and long-term recovery process, potentially contributing to conditions such as Post-Concussion Syndrome (PCS).
Understanding the Blood-Brain Barrier
The blood-brain barrier is a highly selective, semi-permeable membrane composed of tightly packed endothelial cells lining the blood vessels in the brain. Its primary function is to regulate the movement of molecules between the bloodstream and the brain, allowing essential nutrients like glucose and oxygen to pass through while blocking harmful substances, such as toxins and inflammatory agents.
The BBB's selective permeability is crucial for maintaining the brain's delicate balance and protecting it from fluctuations in blood composition that could interfere with neuronal function. It also plays an essential role in preventing immune cells and other potentially harmful agents from entering the brain's extracellular space, which is particularly important in preventing inflammation and damage to neural tissue.
However, when the brain experiences a traumatic event like a concussion, the force of the impact can cause the BBB to become "leaky," allowing substances that are normally kept out of the brain to pass through. This breach in the BBB can lead to neuroinflammation, oxidative stress, and increased vulnerability to additional injuries.
How a Concussion Disrupts the Blood-Brain Barrier
The mechanical forces involved in a concussion can physically damage the endothelial cells that make up the blood-brain barrier. This disruption results in increased permeability, allowing proteins, immune cells, and other molecules that would typically be blocked to enter the brain. One of the most damaging effects of BBB disruption is the entry of pro-inflammatory cytokines, which can trigger widespread inflammation in the brain.
Inflammation is a normal part of the body’s response to injury, but in the brain, excessive or prolonged inflammation can cause further damage to neurons and glial cells. This can contribute to the long-term cognitive and emotional symptoms seen in PCS. Additionally, a leaky BBB allows harmful oxidative agents to accumulate in the brain, leading to oxidative stress. Oxidative stress damages cellular components such as DNA, proteins, and lipids, further impeding the brain’s ability to heal.
A study published in Frontiers in Neuroscience demonstrated that BBB disruption following a traumatic brain injury is closely linked to both acute and chronic neuroinflammation, which can impair cognitive function and lead to long-term brain health issues. The study highlighted that even subtle changes in BBB integrity can have significant consequences for brain recovery, emphasizing the need for strategies to restore and protect the BBB after a concussion.
Consequences of a Compromised Blood-Brain Barrier in Concussion Recovery
When the blood-brain barrier is compromised, the brain becomes vulnerable to a wide range of detrimental processes. The increased permeability of the BBB allows harmful substances, including blood-borne toxins, immune cells, and inflammatory mediators, to infiltrate the brain. This infiltration can lead to several adverse effects that complicate concussion recovery.
1. Neuroinflammation
As mentioned earlier, the breakdown of the BBB allows pro-inflammatory molecules to enter the brain, leading to an exaggerated inflammatory response. Chronic neuroinflammation is a significant factor in the persistence of symptoms seen in PCS, such as headaches, mood disturbances, and cognitive impairments. If neuroinflammation is not addressed, it can lead to neuronal damage and contribute to neurodegenerative processes.
2. Oxidative Stress
BBB disruption also leads to increased oxidative stress in the brain, as harmful free radicals and reactive oxygen species (ROS) are allowed to accumulate. Oxidative stress can damage neuronal structures, including cell membranes and mitochondrial DNA, further impairing brain function. This process is associated with cognitive decline, memory problems, and other long-term effects of concussions.
3. Neurovascular Dysfunction
The BBB is critical for maintaining proper blood flow and nutrient delivery to the brain. When the BBB is compromised, neurovascular dysfunction can occur, leading to reduced cerebral blood flow and impairing the brain's ability to receive adequate oxygen and glucose. This further contributes to the energy crisis that occurs after a concussion and can prolong recovery by limiting the brain's ability to repair itself.
4. Increased Risk of Secondary Injury
A leaky BBB increases the risk of secondary injuries following a concussion. Without the protective barrier intact, the brain is more vulnerable to further trauma and may be less resilient to future concussions or even mild head impacts. This is particularly concerning for athletes or individuals in professions where repeated head injuries are common, as it increases the likelihood of developing chronic traumatic encephalopathy (CTE) or other long-term neurological conditions.
Strategies to Restore and Protect the Blood-Brain Barrier
Given the critical role that the BBB plays in maintaining brain health and facilitating recovery, it is essential to prioritize strategies that restore its integrity and protect it from further damage. Several interventions have shown promise in supporting the BBB and promoting recovery after a concussion.
1. Nutritional Support for BBB Repair
Certain nutrients have been shown to support the integrity of the blood-brain barrier. For example, omega-3 fatty acids, particularly docosahexaenoic acid (DHA), are essential for maintaining the structure of endothelial cells and reducing inflammation. Studies have demonstrated that omega-3 supplementation can help reduce BBB permeability and promote brain recovery following traumatic brain injuries.
In addition to omega-3s, antioxidants such as vitamins C and E play a crucial role in reducing oxidative stress and protecting the BBB from free radical damage. These nutrients help neutralize ROS, reducing the oxidative damage that can further compromise the BBB after a concussion.
2. Non-invasive Therapies
Therapies such as hyperbaric oxygen ketone therapy (HBOKT) and low-level laser therapy (LLLT) have also been shown to enhance the repair of the blood-brain barrier. HBOT increases oxygen delivery to the brain, which supports cellular repair processes and helps reduce inflammation. LLLT stimulates cellular activity and promotes the production of growth factors that aid in the repair of endothelial cells, helping to restore BBB integrity.
3. Physical Exercise
Moderate physical exercise has been shown to improve cerebral blood flow and support BBB health. Regular aerobic exercise can enhance the delivery of oxygen and nutrients to the brain, promoting repair processes and improving overall brain function. However, it is important that exercise be carefully managed following a concussion to avoid exacerbating symptoms.
The Importance of Early Intervention with Carolina Brain Center
As with other aspects of concussion recovery, early intervention is critical when it comes to protecting and repairing the blood-brain barrier. The sooner that strategies to reduce inflammation, oxidative stress, and neurovascular dysfunction are implemented, the better the chances of preventing long-term cognitive and emotional impairments. Healthcare providers should assess BBB integrity as part of the initial concussion evaluation and tailor treatment plans accordingly.
At Carolina Brain Center in Raleigh, NC, we recognize the importance of maintaining and repairing the blood-brain barrier in concussion recovery. Our comprehensive approach includes therapies designed to reduce inflammation, enhance blood flow, and support the brain's natural healing processes. By addressing BBB disruption early, we can help patients recover more effectively and prevent the long-term complications associated with concussions.
If you’re experiencing prolonged concussion symptoms or are concerned about the impact of a recent head injury, contact Carolina Brain Center today. Our personalized treatment plans are designed to promote faster, more complete recovery. Start your journey to healing today—because the right care can make all the difference.
Excitotoxicity and Its Role in Concussion-Induced Neurodegeneration
Concussions are more than just a temporary disruption of brain function. They set off a series of complex biochemical events that can lead to long-term brain damage, especially if left untreated. One of the most significant processes triggered by a concussion is excitotoxicity, a condition where neurons are overstimulated to the point of damage or death. This overstimulation is primarily caused by the excessive release of the neurotransmitter glutamate, which, under normal conditions, helps facilitate communication between neurons.
However, in the aftermath of a concussion, this process goes awry. The brain's inability to regulate glutamate leads to a cascade of events that can result in cell death, contributing to neurodegeneration and long-term cognitive impairment. Excitotoxicity in concussion-induced neurodegeneration has many implications on brain health, but there are strategies to mitigate its damaging effects during recovery.
Understanding Excitotoxicity: The Role of Glutamate
Glutamate is the primary excitatory neurotransmitter in the brain, responsible for sending signals between neurons. Under normal circumstances, the release of glutamate is carefully regulated to ensure that neurons are appropriately stimulated without becoming overexcited. However, after a concussion, the brain experiences a surge in glutamate release. This surge, coupled with the impaired function of glutamate transporters (which normally help remove excess glutamate from the synapses), leads to the accumulation of glutamate in the extracellular space.
This accumulation of glutamate overstimulates neurons by activating glutamate receptors, such as NMDA (N-methyl-D-aspartate) and AMPA receptors. These receptors allow calcium ions (Ca2+) to enter the neurons, leading to a dangerous influx of calcium. While calcium plays an essential role in many cellular processes, excessive calcium within neurons can trigger a chain reaction that damages cell membranes, disrupts mitochondrial function, and activates enzymes that break down proteins and DNA. This process is what ultimately leads to neuronal death—a hallmark of excitotoxicity.
The Consequences of Excitotoxicity in Concussion
In the context of a concussion, excitotoxicity plays a central role in the neurometabolic cascade of concussion that follows the initial mechanical injury. The excessive stimulation of neurons caused by glutamate leads to the production of reactive oxygen species (ROS), which cause oxidative stress. This oxidative stress damages cellular components, including membranes, proteins, and mitochondria, further impairing the brain's ability to recover from the injury.
One of the most concerning consequences of excitotoxicity is its contribution to neurodegeneration. When neurons are damaged or die due to excitotoxicity, the brain's capacity for communication and plasticity is compromised. This can lead to long-term cognitive impairments, such as difficulties with memory, attention, and executive function. In severe cases, excitotoxicity may also contribute to the development of neurodegenerative disorders, such as Alzheimer's and Parkinson's disease, by accelerating the loss of neurons and promoting the accumulation of toxic proteins like beta-amyloid.
Calcium Overload and Mitochondrial Dysfunction
One of the primary mechanisms through which excitotoxicity causes neuronal death is calcium overload. When glutamate receptors are overstimulated, they allow large amounts of calcium to enter neurons. This calcium overload overwhelms the mitochondria, the energy-producing centers of the cell, impairing their ability to produce ATP (adenosine triphosphate). Without sufficient ATP, neurons cannot maintain their normal functions, leading to energy failure and eventual cell death.
Mitochondrial dysfunction caused by calcium overload also contributes to the generation of reactive oxygen species (ROS), which exacerbate oxidative stress and damage cellular components. This creates a vicious cycle where mitochondrial dysfunction and oxidative stress feed into one another, further amplifying the damage caused by excitotoxicity.
Additionally, calcium overload activates enzymes such as calpains and caspases, which break down cellular proteins and contribute to cell death through a process called apoptosis. Apoptosis, or programmed cell death, is a natural process that helps eliminate damaged cells. However, in the case of excitotoxicity, apoptosis is triggered excessively, leading to the loss of healthy neurons.
How Excitotoxicity Contributes to Neurodegeneration
Excitotoxicity doesn't just affect neurons in the immediate aftermath of a concussion. It sets the stage for long-term neurodegeneration, particularly in patients who experience multiple concussions or suffer from Post-Concussion Syndrome (PCS). The chronic effects of excitotoxicity can lead to the accumulation of damaged proteins, the loss of synaptic connections, and the eventual death of neurons, all of which contribute to the progressive decline in brain function.
In some cases, excitotoxicity has been linked to the development of neurodegenerative diseases. For example, research has shown that chronic excitotoxicity can promote the accumulation of beta-amyloid, a protein associated with Alzheimer's disease. Excessive calcium influx and mitochondrial dysfunction also play a role in the development of neurofibrillary tangles, another hallmark of Alzheimer's. Similarly, excitotoxicity has been implicated in the degeneration of dopaminergic neurons in Parkinson's disease.
For patients recovering from concussions, the long-term effects of excitotoxicity may manifest as cognitive decline, memory problems, and difficulty with concentration and decision-making. These symptoms can persist for months or even years, particularly if the excitotoxic cascade is not properly managed during the early stages of recovery.
Strategies to Mitigate Excitotoxicity in Concussion Recovery
Given the significant role that excitotoxicity plays in concussion-induced neurodegeneration, managing this process is critical for improving recovery outcomes and preventing long-term cognitive decline. Several strategies have emerged that focus on reducing glutamate release, protecting neurons from calcium overload, and supporting mitochondrial function.
1. Glutamate Modulation
One of the most effective ways to mitigate excitotoxicity is to reduce the release of glutamate or block its interaction with receptors. Certain nutritional interventions, such as the ketogenic diet, can help regulate glutamate levels in the brain. The ketogenic diet shifts the brain's energy source from glucose to ketones, which have been shown to reduce glutamate release and enhance the production of GABA, a calming neurotransmitter that counteracts the excitatory effects of glutamate.
2. Antioxidant Therapy
Since excitotoxicity generates reactive oxygen species (ROS) that contribute to oxidative stress, antioxidant therapy is a valuable tool for reducing neuronal damage. Antioxidants such as coenzyme Q10 (CoQ10), N-acetylcysteine (NAC), and vitamins C and E can help neutralize ROS and protect neurons from oxidative damage. These supplements support mitochondrial function and reduce the impact of excitotoxicity on long-term brain health.
3. Hyperbaric Oxygen Ketone Therapy (HBOKT)
Hyperbaric Oxygen Ketone Therapy (HBOKT) has been shown to reduce excitotoxicity by increasing oxygen delivery to damaged brain tissues. This therapy enhances mitochondrial function, reduces oxidative stress, and promotes the repair of damaged neurons. HBOT is particularly useful for patients with Post-Concussion Syndrome, as it helps address both the acute and chronic effects of excitotoxicity.
The Importance of Early Intervention
Excitotoxicity begins immediately after a concussion, making early intervention critical for preventing long-term neurodegeneration. The sooner that strategies to mitigate excitotoxicity are implemented, the greater the chances of reducing neuronal damage and improving recovery outcomes. For patients with a history of multiple concussions or those experiencing prolonged symptoms, proactive management of excitotoxicity is especially important for preventing cognitive decline and neurodegenerative diseases.
Have You Experienced a Concussion?
At Carolina Brain Center in Raleigh, NC, we recognize the importance of addressing excitotoxicity in concussion recovery. Our personalized approach integrates therapies such as glutamate modulation, antioxidant support, and hyperbaric oxygen therapy to reduce the effects of excitotoxicity and promote faster recovery.
If you've recently experienced a concussion, don't wait to seek treatment. By addressing excitotoxicity early, we can help prevent long-term cognitive decline and neurodegeneration. Start your recovery journey by filling out our phone consultation request form today. The knowledge and care you receive will set you on the path to healing.