The Potential of Low-Level Laser Therapy (LLLT) in Treating Concussions
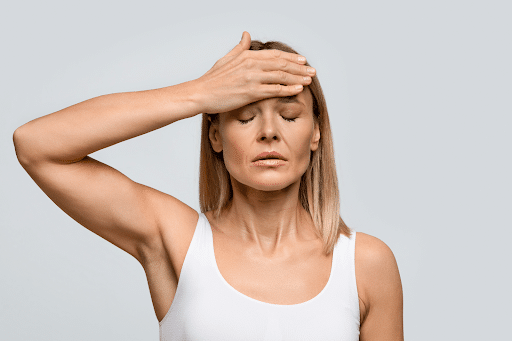
 Concussions are increasingly recognized as complex injuries that extend beyond immediate symptoms like headaches and dizziness. At the cellular level, a concussion triggers a cascade of biochemical processes, including inflammation, oxidative stress, and mitochondrial dysfunction. These processes not only contribute to the acute phase of injury but can also prolong symptoms, leading to conditions like Post-Concussion Syndrome (PCS). As research progresses, new therapeutic approaches are emerging that target the underlying cellular damage caused by concussions. One such therapy is Low-Level Laser Therapy (LLLT), a non-invasive treatment that uses light energy to stimulate cellular repair and promote healing.
Concussions are increasingly recognized as complex injuries that extend beyond immediate symptoms like headaches and dizziness. At the cellular level, a concussion triggers a cascade of biochemical processes, including inflammation, oxidative stress, and mitochondrial dysfunction. These processes not only contribute to the acute phase of injury but can also prolong symptoms, leading to conditions like Post-Concussion Syndrome (PCS). As research progresses, new therapeutic approaches are emerging that target the underlying cellular damage caused by concussions. One such therapy is Low-Level Laser Therapy (LLLT), a non-invasive treatment that uses light energy to stimulate cellular repair and promote healing.
Let’s explore how LLLT works to treat concussions, its potential benefits in accelerating recovery, and the evidence supporting its use. By addressing the root causes of concussion symptoms, LLLT offers a promising option for patients seeking relief from both acute and prolonged symptoms.
How LLLT Works: Mechanisms of Action
LLLT, also known as photobiomodulation, uses light in the near-infrared spectrum to penetrate the scalp and interact with cellular structures in the brain. The therapy specifically targets mitochondria, the energy-producing centers of the cell. Mitochondria contain a protein called cytochrome c oxidase, which absorbs light and uses the energy to increase ATP (adenosine triphosphate) production. ATP is essential for powering cellular functions, and its production is often impaired after a concussion due to mitochondrial dysfunction.
By boosting ATP production, LLLT helps restore the energy balance in neurons, enabling them to function more effectively and repair damage. In addition to increasing energy production, LLLT also has anti-inflammatory effects. It reduces the release of pro-inflammatory cytokines, molecules that contribute to the chronic inflammation often seen in patients with PCS. Furthermore, LLLT stimulates the release of antioxidants, which neutralize harmful reactive oxygen species (ROS) produced during the injury, reducing oxidative stress and preventing further cellular damage.
One of the most significant advantages of LLLT is its ability to promote neuroplasticity—the brain’s ability to adapt and reorganize itself. LLLT has been shown to enhance synaptogenesis (the formation of new synapses between neurons) and neurogenesis (the growth of new neurons), both of which are critical for cognitive recovery following a concussion.
The Benefits of LLLT for Concussion Recovery
1. Reducing Inflammation
Inflammation is a natural response to brain injury, but when it becomes chronic, it can impede recovery and contribute to long-term symptoms. Patients with PCS often experience neuroinflammation, which can manifest as cognitive deficits, mood disturbances, and physical symptoms like headaches and fatigue. LLLT helps reduce this inflammation by downregulating pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6).
By reducing inflammation, LLLT alleviates many of the persistent symptoms associated with PCS. Research has shown that patients treated with LLLT experience faster resolution of symptoms and an improved ability to return to normal activities. This is particularly important for patients who suffer from prolonged symptoms and have been unable to find relief through conventional treatments.
2. Enhancing Mitochondrial Function
Mitochondrial dysfunction is a hallmark of the neurometabolic cascade triggered by a concussion. When mitochondria are damaged, they cannot produce sufficient ATP to meet the brain’s energy demands, leading to cognitive fatigue, memory problems, and difficulty concentrating. LLLT directly targets mitochondria, increasing their ability to produce ATP and repair damage.
Enhanced mitochondrial function allows neurons to recover more effectively and regain their normal function. This improvement in cellular energy production is key to reducing cognitive symptoms and improving overall brain health. For patients with PCS, LLLT offers a way to restore energy balance in the brain, which can accelerate recovery and prevent the progression of long-term neurological issues.
3. Stimulating Neuroplasticity
One of the most exciting aspects of LLLT is its ability to promote neuroplasticity. After a concussion, the brain often struggles to form new connections and repair damaged neural pathways. This can lead to persistent cognitive deficits and impairments in memory, attention, and problem-solving skills. LLLT stimulates the release of growth factors, such as brain-derived neurotrophic factor (BDNF), which support the growth of new neurons and the formation of new synapses.
By promoting neuroplasticity, LLLT helps the brain adapt and recover from the damage caused by a concussion. Patients treated with LLLT often report improvements in cognitive function, including better memory retention, faster processing speeds, and enhanced attention. These benefits make LLLT a valuable tool for both short-term recovery and long-term brain health.
Scientific Evidence Supporting LLLT in Concussion Treatment
In clinical trials, patients treated with LLLT reported a reduction in headaches, improved cognitive function, and better overall quality of life compared to those who received standard treatments. These findings are particularly encouraging for patients with PCS, who often experience lingering symptoms that are difficult to treat with conventional therapies.
A study published in Photomedicine and Laser Surgery explored the effects of LLLT on patients with mild traumatic brain injuries, including concussions. The researchers found that LLLT reduced inflammation and oxidative stress, while also improving cognitive performance and mood. The study emphasized the importance of early intervention with LLLT to prevent the progression of long-term symptoms.
Combining LLLT with Other Therapies
While LLLT is a powerful tool in concussion recovery, its benefits are often maximized when combined with other therapeutic interventions. For example, Hyperbaric Oxygen Keotne Therapy (HBOT) can be used alongside LLLT to enhance oxygen delivery to the brain, further improving mitochondrial function and reducing inflammation. Nutritional interventions, such as the ketogenic diet, can also support mitochondrial health by providing the brain with an alternative energy source (ketones), which may improve the overall effectiveness of LLLT.
Physical therapy and cognitive rehabilitation are also important components of a comprehensive treatment plan for concussion recovery. LLLT can accelerate the brain’s ability to form new neural connections, making it easier for patients to benefit from cognitive training and physical therapy exercises. By combining these therapies, healthcare providers can offer a holistic approach that addresses the full spectrum of concussion symptoms.
Safety and Accessibility of LLLT
One of the most attractive features of LLLT is its safety profile. Unlike invasive treatments or medications, LLLT is non-invasive and has few, if any, side effects. Patients typically tolerate the therapy well, and the sessions are painless. LLLT can be performed in an outpatient setting, making it accessible to patients who may not require hospitalization but still need targeted therapy for concussion recovery.
While more research is needed to fully understand the long-term effects of LLLT, the current evidence suggests that it is a safe and effective option for managing both acute and prolonged concussion symptoms. Its ability to target the underlying causes of these symptoms makes it a valuable addition to any concussion treatment plan.
Carolina Brain Center Can Help In Your Recovery Process
At Carolina Brain Center in Raleigh, NC, we believe in using cutting-edge therapies like Low-Level Laser Therapy (LLLT) to help patients recover from concussions more quickly and effectively. LLLT addresses the root causes of concussion symptoms by improving mitochondrial function, reducing inflammation, and promoting neuroplasticity. Whether you're dealing with acute symptoms or long-term effects like Post-Concussion Syndrome, LLLT administered by Dr. Dane at Carolina Brain Center can help accelerate your recovery and restore your quality of life.
If you've experienced a concussion and are looking for innovative, non-invasive treatments, Carolina Brain Center can help. Start your recovery journey today by filling out our consultation request form. The vast knowledge and care you receive in our clinic will set you on the path to healing.
Ketogenic Diet as a Therapeutic Strategy for Concussion Recovery

Traumatic brain injuries (TBIs), including concussions, are becoming increasingly recognized for their long-term effects on cognitive function, mood, and overall brain health. When a person experiences a concussion, the immediate focus is often on physical symptoms such as headaches, dizziness, and confusion. However, the underlying biochemical changes in the brain—the neurometabolic cascade of concussion—can persist well after the initial injury, leading to prolonged symptoms. Recent research has explored alternative therapeutic strategies to support brain recovery, and one of the most promising interventions is the ketogenic diet. By providing an alternative energy source to glucose, which is often impaired after a brain injury, the ketogenic diet may help resolve the energy crisis and oxidative stress triggered by the neurometabolic cascade of concussion.
Understanding the Neurometabolic Cascade of Concussion
When a concussion occurs, the brain undergoes a complex set of biochemical reactions known as the neurometabolic cascade of concussion (NMCC). This cascade is triggered by the initial mechanical forces that disrupt neuronal function, leading to excitotoxicity (excessive neuronal firing), oxidative stress, and impaired glucose metabolism. These changes result in a brain-wide energy crisis where neurons struggle to maintain homeostasis, leading to cognitive, emotional, and physical impairments.
The cascade begins with the release of excitatory neurotransmitters such as glutamate, leads to a massive efflux of potassium out of the cells creating a higher demand for ATP (the cells’ energy currency) within a disrupted supply chain. Because the NMCC also leads to calcium influx into cells, the mitochondrial—the powerhouse of the cell—struggles to keep up with the supply needed to meet the new higher demand. Mitochondrial dysfunction is one of the critical drivers of the brain's energy crisis post-concussion.
In 2001, Giza and Hovda introduced the concept of the neurometabolic cascade, emphasizing that the secondary injuries following the initial trauma, such as oxidative stress and inflammation, contribute to long-term neurological deficits. These secondary injuries can persist for weeks, months, or even years, highlighting the importance of addressing the cascade early on to prevent chronic symptoms.
Ketones as an Alternative Energy Source for the Brain
The ketogenic diet, which involves drastically reducing carbohydrate intake and increasing fat consumption, forces the body to switch from using glucose as its primary fuel source to using ketones. Ketones, such as beta-hydroxybutyrate (BHB) and acetoacetate (AcAc), are produced by the liver during periods of fasting or carbohydrate restriction. These ketones serve as an alternative energy source for the brain, bypassing the glucose metabolism pathways that are often impaired after a concussion.
Research published by the NIH has shown that ketone bodies provide a more efficient and stable source of energy for the brain compared to glucose. In a concussed brain, where glucose metabolism is impaired due to mitochondrial dysfunction and reduced cerebral blood flow, ketones offer a critical alternative fuel that can help restore energy balance and support recovery. Ketones are readily used by neurons and other brain cells, enhancing mitochondrial function and reducing oxidative stress.
In a 2021 review, NIH researchers highlighted the neuroprotective properties of ketones in conditions of traumatic brain injury. They found that ketones not only provide an alternative source of ATP but also reduce the production of reactive oxygen species (ROS), molecules that contribute to cellular damage and inflammation after a concussion. By reducing oxidative stress, ketones can help protect the brain from further injury and promote cellular repair.
The Role of Ketones in Reducing Excitotoxicity and Inflammation
Excitotoxicity, which occurs when neurons are overstimulated by excessive amounts of glutamate, is one of the main contributors to neuronal damage after a concussion. Glutamate, an excitatory neurotransmitter, is released in large quantities following brain trauma and overstimulates neurons, leading to calcium influx into cells. This calcium overload damages mitochondria, resulting in further energy deficits and ultimately, cell death. The ketogenic diet has been shown to modulate this process by increasing the production of gamma-aminobutyric acid (GABA), a calming neurotransmitter that counteracts the effects of glutamate.
According to a study published in Frontiers in Neurology, ketone bodies can reduce excitotoxicity by enhancing GABA activity and limiting glutamate release. This reduction in neuronal firing prevents further neuronal damage and allows the brain to recover from the excitotoxic effects of the neurometabolic cascade. Additionally, ketones have been shown to stabilize neuronal membranes and improve the function of ion channels, which are critical for maintaining cellular homeostasis in the aftermath of a concussion.
Inflammation is another key factor in the progression of post-concussion symptoms. Chronic inflammation in the brain, driven by the release of pro-inflammatory cytokines, contributes to the development of conditions such as post-concussion syndrome (PCS), characterized by persistent symptoms like headaches, dizziness, and cognitive impairments. The ketogenic diet, through its anti-inflammatory effects, has been shown to reduce the levels of these cytokines, including tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6), which are elevated after a traumatic brain injury.
A review conducted by the NIH in 2022 highlighted that ketone bodies can downregulate inflammatory pathways in the brain, thereby reducing the risk of developing chronic neuroinflammation. This reduction in inflammation not only accelerates recovery but also decreases the risk of long-term complications such as depression, anxiety, and even neurodegenerative diseases like Alzheimer's.
Clinical Evidence Supporting the Ketogenic Diet in Concussion Recovery
While most of the research on the ketogenic diet has focused on epilepsy, its potential benefits for brain injury recovery are gaining increasing attention. Clinical studies have begun to explore the effects of ketosis on cognitive function, inflammation, and energy metabolism in individuals recovering from concussions. The NIH has supported several studies that suggest ketones can enhance recovery following brain injury by providing the brain with an alternative fuel source and protecting against further damage.
A study published in Journal of Neurotrauma, researchers examined the effects of a ketogenic diet on cognitive function in patients with mild traumatic brain injury. The results showed that patients who followed a ketogenic diet demonstrated significant improvements in memory, attention, and overall cognitive performance compared to those who consumed a standard diet. The study also found that ketogenic patients had lower levels of oxidative stress and inflammation, indicating that the diet had a protective effect on the brain.
Additionally, a study published in Frontiers in Nutrition highlighted the ability of ketones to reduce brain edema (swelling) and improve mitochondrial function following brain trauma. These findings provide further support for the use of the ketogenic diet in concussion recovery, as brain swelling and mitochondrial dysfunction are common issues that hinder recovery. The researchers concluded that the ketogenic diet not only provides neuroprotection but also enhances the brain’s capacity for healing by supporting cellular repair mechanisms.
Implementing the Ketogenic Diet in Clinical Practice
While the ketogenic diet holds promise as a therapeutic tool for concussion recovery, it is essential to approach its implementation with care. Transitioning to a state of ketosis requires strict dietary modifications that involve reducing carbohydrate intake to less than 10% of daily calories and increasing fat intake to 70-80%. This shift can be challenging for some patients, especially those unfamiliar with low-carbohydrate diets.
In clinical practice, the ketogenic diet should be implemented under the guidance of healthcare professionals who can monitor patients for potential side effects such as fatigue, dehydration, or electrolyte imbalances. It is important to ensure that patients remain well-hydrated and consume adequate amounts of electrolytes (such as sodium, potassium, and magnesium) to prevent complications. Additionally, exogenous ketones, which are ketone supplements, may be used to help patients achieve ketosis more quickly, especially in the acute phase of concussion recovery.
Healthcare providers should also consider combining the ketogenic diet with other therapeutic interventions, such as hyperbaric oxygen therapy (HBOT) or transcranial low-level laser therapy (LLLT), to maximize recovery outcomes. By addressing both the neurometabolic and physical aspects of concussion recovery, a comprehensive approach can be developed that supports the patient’s overall well-being.
Addressing Post-Concussion Syndrome (PCS) with Ketosis
For individuals suffering from post-concussion syndrome (PCS), where symptoms persist beyond the typical recovery period, the ketogenic diet may offer an additional benefit. Chronic inflammation and ongoing oxidative stress are significant contributors to PCS, and ketones can help reduce these processes.
Because ketones provide a stable source of energy for the brain, they help alleviate the "brain fog" and cognitive fatigue often reported by PCS patients. This improvement in mental clarity is likely due to the reduction in neuroinflammation and oxidative damage, allowing the brain to heal more effectively.
How We Can Help
At Carolina Brain Center in Raleigh, NC, we believe that understanding the neurometabolic cascade and using innovative treatments can accelerate concussion recovery. Our personalized approach from both in-office treatments and at-home work incorporates therapies like the ketogenic diet, hyperbaric oxygen therapy, and transcranial low-level laser therapy to help patients heal efficiently.
If you’ve recently experienced a concussion and feel too unwell to start treatment, we offer strategies that allow you to begin healing even while resting. For acute concussions, we use a combination of hyperbaric oxygen ketone therapy and laser therapy to reduce the effects of the neurometabolic cascade. For patients with prolonged symptoms, we develop customized rehabilitation programs that combine at-home and in-office treatments.
Take the first step towards recovery by filling out our phone consultation request form today. The knowledge and care you'll receive at Carolina Brain Center will set you on the path to healing.
The Role of Mitochondrial Dysfunction in Post-Concussion Syndrome
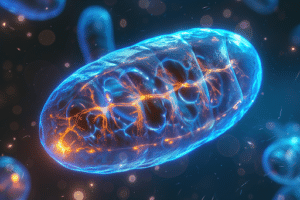
Concussions are often thought of as temporary injuries, with symptoms that resolve within days or weeks. However, for many individuals, concussions can have lingering effects that last for months or even years, a condition known as Post-Concussion Syndrome (PCS). One of the key mechanisms driving the long-term effects of PCS is mitochondrial dysfunction. Mitochondria, often referred to as the "powerhouses" of the cell, are responsible for producing energy in the form of ATP (adenosine triphosphate). When a concussion occurs, the delicate balance within mitochondria is disrupted, leading to a cascade of problems that contribute to the persistent symptoms of PCS.
This article explores the critical role that mitochondrial dysfunction plays in PCS, examining the scientific evidence behind this phenomenon and the potential strategies for addressing it during recovery. A comprehensive understanding of mitochondrial health can offer new pathways for treatment, both in the acute phase of injury and in long-term care.
Understanding Mitochondrial Dysfunction After a Concussion
When the brain experiences trauma, such as a concussion, neurons undergo significant metabolic stress. The initial mechanical damage leads to a surge in calcium ions within neurons, which overwhelms the mitochondria. Mitochondria are tasked with regulating calcium levels within the cell, but this sudden influx impairs their function. As a result, mitochondria cannot produce ATP as efficiently, and they generate higher levels of reactive oxygen species (ROS), molecules that cause oxidative damage to cells.
This combination of reduced energy production and increased oxidative stress leads to further cellular damage and dysfunction. The mitochondria, which are critical for sustaining cellular activity, become a source of cellular stress and inflammation. This dysfunction is not limited to the acute phase of the injury. Long after the initial impact, mitochondrial damage can persist, contributing to chronic symptoms such as cognitive difficulties, fatigue, headaches, and mood disturbances—all hallmark signs of PCS.
A study published by the National Institutes of Health (NIH) supports this understanding, showing that mitochondrial dysfunction plays a central role in the neurometabolic cascade of concussion. The research highlights that disruptions in mitochondrial function not only impair energy production but also contribute to long-term neuroinflammation, which underpins many of the symptoms seen in PCS.
The Neurometabolic Cascade and Its Impact on Mitochondria
Following a concussion, the brain undergoes a series of biochemical changes referred to as the neurometabolic cascade of concussion. This cascade begins with the release of excitatory neurotransmitters like glutamate, which creates a massive efflux of potassium out of the cells. This creates a larger demand for ATP, the cells energy currency, and ultimately leads to an energy crisis. Moreover, there is a massive influx of calcium into the cells. Mitochondria, responsible for buffering calcium within cells, are quickly overwhelmed by this surge. In a healthy state, mitochondria produce ATP through oxidative phosphorylation, a process that requires tight regulation of calcium levels. However, in the concussed brain, mitochondrial membranes are disrupted, leading to a loss of control over calcium homeostasis and ultimately cannot keep up with the new demand for energy, ATP, and the energy crisis becomes an even bigger problem.
This mitochondrial stress results in the production of reactive oxygen species (ROS), which cause oxidative damage to both the mitochondria and surrounding cellular structures. Over time, these oxidative damage compounds further impair mitochondrial function and exacerbate the energy crisis within neurons. Without sufficient energy, neurons struggle to carry out their essential functions, leading to symptoms such as cognitive impairment, mood disturbances, and fatigue, which are often observed in patients with PCS.
The persistent nature of mitochondrial dysfunction is what makes PCS so challenging to treat. While many symptoms of concussion resolve within a few weeks, mitochondrial damage can linger, creating a cycle of ongoing cellular stress and neuroinflammation that prolongs recovery.
How Mitochondrial Dysfunction Contributes to Post-Concussion Symptoms
One of the most significant ways mitochondrial dysfunction affects patients with PCS is through its impact on energy metabolism. The brain is an energy-intensive organ, and when it cannot produce enough ATP, cognitive function, memory, and mood regulation are all affected. Patients with PCS often report "brain fog," difficulty concentrating, and memory lapses—all of which are likely tied to the brain's reduced ability to meet its energy demands.
In addition to cognitive symptoms, mitochondrial dysfunction also contributes to physical symptoms such as headaches and fatigue. This is because mitochondria are also involved in regulating the function of blood vessels and the autonomic nervous system, which controls involuntary processes such as heart rate and blood pressure. When mitochondrial function is impaired, blood flow to the brain can be disrupted, leading to symptoms such as headaches, dizziness, and light sensitivity, which are commonly seen in PCS patients.
Furthermore, mitochondrial dysfunction plays a critical role in maintaining the balance of neurotransmitters, the chemicals that transmit signals between neurons. When mitochondria are damaged, they are unable to efficiently recycle neurotransmitters, leading to imbalances that can affect mood and emotional regulation. Many patients with PCS experience symptoms of anxiety, depression, and irritability, which are thought to be related to these neurotransmitter imbalances.
Addressing Mitochondrial Dysfunction in Post-Concussion Care
Given the central role that mitochondrial dysfunction plays in PCS, addressing this issue is key to effective treatment. Several strategies have emerged that focus on restoring mitochondrial health and improving energy production in the brain. One of the most promising approaches is the use of antioxidant therapy. Antioxidants help neutralize the reactive oxygen species that are produced by damaged mitochondria, reducing oxidative stress and preventing further damage.
A study published in the Journal of Neurotrauma explored the use of antioxidants such as coenzyme Q10 (CoQ10) and N-acetylcysteine (NAC) in patients with brain injuries. The findings showed that these compounds could improve mitochondrial function, reduce oxidative stress, and accelerate recovery in patients with PCS. These antioxidants work by supporting the mitochondria's ability to produce ATP and by preventing the accumulation of oxidative damage that impairs cellular function.
Another approach to addressing mitochondrial dysfunction involves optimizing energy production through nutritional interventions. The ketogenic diet, which shifts the brain's energy source from glucose to ketones, has shown promise in improving mitochondrial function. Ketones are a more efficient fuel source for the brain and can bypass some of the metabolic impairments caused by mitochondrial damage. Research suggests that the ketogenic diet may help reduce symptoms of PCS by providing the brain with an alternative energy source and supporting mitochondrial recovery.
Physical therapies, such as hyperbaric oxygen ketone therapy (HBOKT) and transcranial low-level laser therapy (LLLT), have also been explored as methods for improving mitochondrial function. HBOKT increases the availability of oxygen in the brain, which enhances mitochondrial respiration and supports ATP production. TLLLT, on the other hand, uses light energy to stimulate mitochondrial activity and reduce inflammation. Both therapies have been studied for their potential to accelerate recovery in patients with PCS, with promising results.
The Importance of Early Intervention
Mitochondrial dysfunction begins immediately after a concussion, making early intervention critical to preventing long-term damage. The sooner therapies targeting mitochondrial health are implemented, the greater the chances of preventing the development of PCS. For example, initiating antioxidant therapy or hyperbaric oxygen ketone therapy shortly after the injury can help stabilize mitochondrial function and prevent the cascade of oxidative stress and inflammation that contributes to prolonged symptoms.
Early intervention is also important for patients who are at higher risk of developing PCS, such as those with a history of multiple concussions or individuals with pre-existing neurological conditions. In these cases, proactive management of mitochondrial dysfunction may help reduce the severity of symptoms and shorten recovery times.
Carolina Brain Center Can Help
At Carolina Brain Center in Raleigh, NC, we understand the importance of addressing mitochondrial dysfunction in patients recovering from concussions. Our approach combines innovative therapies like hyperbaric oxygen ketone therapy, antioxidant treatments, and personalized rehabilitation programs to help patients recover faster and more effectively.
If you've recently experienced a concussion, don't wait to seek treatment. Our therapies can help address the underlying causes of your symptoms, including mitochondrial dysfunction. For patients dealing with prolonged symptoms, we offer individualized treatment plans that combine in-office therapies with at-home strategies to optimize recovery.
Start your journey to recovery today, with Dr. Dane and the Carolina Brain Center. Complete our phone consultation request form today and let us show you how to start living a pain free life again.
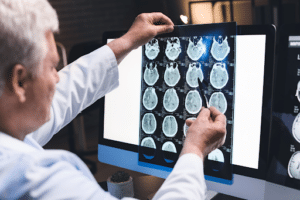
The Importance of Early Intervention in Preventing Long-Term Cognitive Deficits After Concussion
 Concussions, often referred to as mild traumatic brain injuries (mTBIs), are commonly seen in contact sports, motor vehicle accidents, and falls. While they are labeled "mild" due to the absence of structural damage visible on standard brain imaging, concussions can have long-term consequences if not properly addressed. The neurometabolic cascade triggered by the concussion results in complex biochemical changes that, if left untreated, can lead to cognitive deficits, mood disorders, and other lasting impairments. Early intervention following a concussion is critical to preventing these long-term issues.
Concussions, often referred to as mild traumatic brain injuries (mTBIs), are commonly seen in contact sports, motor vehicle accidents, and falls. While they are labeled "mild" due to the absence of structural damage visible on standard brain imaging, concussions can have long-term consequences if not properly addressed. The neurometabolic cascade triggered by the concussion results in complex biochemical changes that, if left untreated, can lead to cognitive deficits, mood disorders, and other lasting impairments. Early intervention following a concussion is critical to preventing these long-term issues.
This article explores the significance of early intervention in managing concussions, emphasizing how prompt and proactive treatment strategies can mitigate the risk of developing long-term cognitive impairments. It also highlights key research supporting the efficacy of early interventions.
The Neurometabolic Cascade and Cognitive Impairments
The brain is particularly vulnerable to the effects of a concussion due to the biochemical changes that occur immediately after impact. The neurometabolic cascade, a process characterized by the release of excitatory neurotransmitters, mitochondrial dysfunction, and oxidative stress, sets the stage for both short- and long-term damage. This cascade results in an energy crisis in the brain, where neurons struggle to generate sufficient ATP (adenosine triphosphate) to function properly. The energy crisis is exacerbated by calcium influx into cells, further damaging mitochondria and impairing cellular function.
In the days following a concussion, the brain remains in a state of heightened vulnerability, particularly to secondary injuries. During this time, the risk of developing long-term cognitive deficits, such as memory problems, reduced attention span, and difficulties with executive function, increases significantly. Research has shown that individuals who do not receive proper intervention in the acute phase of injury are more likely to experience persistent cognitive impairments months or even years later.
The effects of these impairments can range from subtle to profound. Many patients with Post-Concussion Syndrome (PCS) report difficulties with concentration, memory, and problem-solving, all of which can significantly impact daily life and occupational performance. Early intervention aims to disrupt this cascade of damage and provide the brain with the support it needs to heal before long-term effects take hold.
Why Early Intervention is Critical
The first 24 to 72 hours after a concussion are crucial for preventing long-term cognitive deficits. This window represents a period when the brain is most vulnerable but also most responsive to therapeutic interventions. The goal of early intervention is to address the neurometabolic cascade before the brain sustains lasting damage. Without treatment, the inflammatory and oxidative processes initiated by the cascade can cause irreversible harm to neuronal structures, leading to persistent cognitive and emotional impairments.
A study published by the National Institutes of Health (NIH) in 2021 emphasizes the importance of initiating treatment as soon as possible following a concussion. The study found that patients who received early intervention within the first 48 hours of injury had significantly better cognitive outcomes compared to those who delayed treatment. Early intervention was shown to reduce the duration and severity of symptoms, improve cognitive function, and lower the risk of developing chronic neuroinflammation.
Therapeutic Approaches to Early Intervention
1. Rest and Gradual Resumption of Activity
One of the earliest interventions recommended for concussions is cognitive and physical rest. This allows the brain time to recover from the initial injury without added strain. Patients are typically advised to avoid activities that require intense mental effort, such as studying, reading, or screen time, as well as strenuous physical activities. However, prolonged rest beyond 48 hours may delay recovery, so it is crucial to gradually reintroduce light physical and cognitive activities under the guidance of a healthcare professional.
Research has shown that controlled reintroduction of light aerobic exercise can improve cerebral blood flow and help regulate the autonomic nervous system, both of which are disrupted by concussion. This gradual increase in activity promotes neuroplasticity, the brain's ability to reorganize and form new neural connections, which is essential for cognitive recovery.
2. Nutritional Interventions
Nutritional strategies can also play a significant role in early intervention for concussion recovery. Proper nutrition supports mitochondrial function, reduces inflammation, and provides the brain with the nutrients necessary for cellular repair. Omega-3 fatty acids, for example, have been shown to reduce neuroinflammation and improve synaptic plasticity, both of which are critical for cognitive recovery.
Researchers found that supplementation with omega-3 fatty acids in the acute phase of a concussion resulted in improved cognitive function and reduced symptoms of depression and anxiety. Similarly, the ketogenic diet, which shifts the brain's energy source from glucose to ketones, may offer neuroprotective benefits by providing an alternative energy source to support mitochondrial health.
3. Hyperbaric Oxygen Ketone Therapy (HBOKT)
Hyperbaric Oxygen Ketone Therapy (HBOKT) is another intervention that has shown promise in early concussion treatment. By delivering high concentrations of oxygen to the brain, HBOT promotes healing by increasing oxygen availability in areas affected by reduced cerebral blood flow and mitochondrial dysfunction. The NIH has published several studies supporting the use of HBOT to reduce inflammation and enhance cognitive function in patients with mTBI.
HBOT has been shown to improve cognitive recovery by promoting mitochondrial function and reducing oxidative stress. It also accelerates the repair of damaged neuronal pathways, which is critical for restoring cognitive function after a concussion.
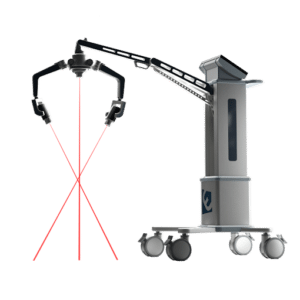
4. Low-Level Laser Therapy (LLLT)
Low-Level Laser Therapy (LLLT), also known as photobiomodulation, uses light energy to stimulate cellular repair and improve mitochondrial function. LLLT has been shown to reduce neuroinflammation, enhance synaptic plasticity, and promote the growth of new neurons (neurogenesis). These effects are particularly beneficial for patients with concussions, as they address both the acute and long-term aspects of brain recovery.
LLLT can significantly improve cognitive performance and reduce the duration of symptoms in patients who receive treatment in the acute phase of injury. The light energy penetrates the scalp and is absorbed by mitochondria in brain cells, stimulating ATP production and reducing oxidative stress, which accelerates recovery.
At Carolina Brain Center, we specialize in using the Erchonia Laser to treat our patients. The Erchonia laser promotes science-backed healing in concussion patients. This non-invasive treatment not only enhances mitochondrial function, but improves cerebral blood flow, and accelerates recovery from concussion-related symptoms such as headaches, cognitive impairment, and dizziness.This laser is one of the many ways that we implement a multipoint approach to concussion care.
The Role of Education in Early Intervention
In addition to medical interventions, education is a key component of early concussion management. Patients and their families should be informed about the risks associated with concussions and the importance of seeking early treatment. Many individuals are unaware of the long-term cognitive risks associated with concussions and may not seek medical attention unless symptoms become severe. Educating patients about the neurometabolic cascade and the potential for long-term damage can encourage them to pursue early interventions that may prevent lasting cognitive deficits.
Healthcare providers should also emphasize the importance of follow-up care. Concussions are dynamic injuries, and symptoms can evolve over time. Regular follow-up appointments allow healthcare professionals to monitor recovery, adjust treatment plans, and address any emerging cognitive or emotional issues.
Our Approach in Early Intervention of Concussion Injury
At Carolina Brain Center in Raleigh, NC, we understand the importance of early intervention in concussion recovery. By addressing the neurometabolic cascade and preventing long-term damage, we help patients recover faster and with fewer lasting effects. Our personalized approach integrates therapies such as low-level laser therapy, hyperbaric oxygen ketone therapy, and nutritional interventions to provide a comprehensive recovery plan.
If you’ve recently suffered a concussion, don’t wait to seek treatment. Early intervention is key to preventing long-term cognitive deficits. At Carolina Brain Center, we are committed to helping you recover fully and efficiently. To start the conversation, contact us today. The knowledge and care you receive will put you on the path to a faster, healthier recovery.
Inflammation and the Brain: How Neuroinflammation Contributes to Prolonged Concussion Symptoms
 Concussions, often described as mild traumatic brain injuries (mTBIs), are far more complex than they appear. Beyond the immediate physical symptoms like headaches, dizziness, and confusion, concussions initiate a series of biochemical processes that can have long-lasting effects on brain health. One of the most significant of these processes is neuroinflammation. This inflammatory response, triggered by the initial injury, is a key driver of the prolonged symptoms seen in conditions like Post-Concussion Syndrome (PCS).
Concussions, often described as mild traumatic brain injuries (mTBIs), are far more complex than they appear. Beyond the immediate physical symptoms like headaches, dizziness, and confusion, concussions initiate a series of biochemical processes that can have long-lasting effects on brain health. One of the most significant of these processes is neuroinflammation. This inflammatory response, triggered by the initial injury, is a key driver of the prolonged symptoms seen in conditions like Post-Concussion Syndrome (PCS).
Neuroinflammation plays a crucial role in determining how well, or how poorly, a patient recovers from a concussion. When the inflammatory response becomes chronic, it can impair cognitive function, contribute to mood disorders, and exacerbate physical symptoms.
What Happens During Neuroinflammation?
When a concussion occurs, the brain experiences a mechanical force that damages neurons and disrupts the blood-brain barrier. This initial trauma sets off an immune response involving the activation of microglia, the brain’s resident immune cells. These microglia release pro-inflammatory cytokines, which are signaling molecules that trigger inflammation. While inflammation is a necessary part of the healing process, it can become problematic when it continues long after the initial injury.
In a healthy response, inflammation helps to clear damaged cells and promote tissue repair. However, in the case of concussions, this process can spiral out of control, leading to a state of chronic inflammation. Microglial cells remain activated for extended periods, continually releasing pro-inflammatory cytokines that contribute to ongoing brain dysfunction. This chronic state of inflammation can impair neuronal communication, disrupt synaptic plasticity (the brain’s ability to adapt and reorganize), and create an environment where cognitive deficits, mood disturbances, and physical symptoms persist.
A study by the National Institutes of Health (NIH) highlights the importance of understanding this prolonged inflammatory response. Researchers have identified that individuals with elevated levels of cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha), are more likely to experience prolonged symptoms after a concussion.
The Role of Inflammatory Cytokines in Post-Concussion Syndrome (PCS)
Cytokines are critical players in the body’s immune response, acting as messengers that regulate inflammation and immune function. Following a concussion, the release of pro-inflammatory cytokines is intended to initiate healing. However, when these cytokines remain elevated for too long, they contribute to ongoing neuroinflammation, which can manifest as cognitive impairment, emotional instability, and persistent physical symptoms.
One of the key cytokines involved in neuroinflammation is IL-6. This cytokine is responsible for both promoting and regulating the inflammatory response. In the context of a concussion, elevated IL-6 levels have been linked to prolonged cognitive deficits, such as difficulties with memory, attention, and executive function. Additionally, increased IL-6 levels can contribute to mood disturbances, including anxiety and depression, both of which are common in patients with PCS.
TNF-alpha is another critical cytokine involved in neuroinflammation. It plays a central role in regulating the immune response and can exacerbate neuronal damage if left unchecked. Elevated TNF-alpha levels following a concussion have been associated with persistent headaches, cognitive decline, and neurodegenerative processes. Chronic elevation of TNF-alpha can also lead to a breakdown of the blood-brain barrier, allowing harmful substances to enter the brain and further contribute to neuroinflammation.
How Neuroinflammation Affects Cognitive Function
Neuroinflammation has a profound impact on cognitive function. The brain’s ability to process information, store memories, and regulate attention is highly dependent on the health of its neurons and synaptic connections. Chronic inflammation disrupts these processes by damaging neurons and impairing synaptic plasticity. This means that the brain is less able to adapt, learn, and repair itself following injury.
Studies have shown that patients with PCS often experience "brain fog," which is characterized by difficulty concentrating, slower processing speeds, and impaired memory. These cognitive deficits can persist for months or even years if the underlying neuroinflammation is not addressed. Inflammation in the hippocampus, a brain region essential for memory formation, has been particularly implicated in the cognitive decline seen in PCS patients. Additionally, neuroinflammation can interfere with neurotransmitter systems, such as the balance between glutamate and GABA, further impairing cognitive function and contributing to mood disorders.
Managing and Reducing Neuroinflammation Post-Concussion
Given the significant role that neuroinflammation plays in prolonging concussion symptoms, addressing inflammation is a key component of effective treatment. Several strategies have emerged to help manage and reduce inflammation, promoting faster recovery and reducing the risk of long-term complications.
1. Nutritional Interventions
Dietary interventions can play a significant role in reducing neuroinflammation. Omega-3 fatty acids, commonly found in fish oil, have been shown to reduce the production of pro-inflammatory cytokines and support neuronal health. A recent study found that patients with brain injuries who supplemented with omega-3 fatty acids experienced reduced neuroinflammation and improved cognitive outcome.
Additionally, antioxidants, such as vitamins C and E, can help neutralize the reactive oxygen species (ROS) produced during the inflammatory response. These antioxidants support mitochondrial function and reduce oxidative stress, both of which are important for maintaining cognitive function post-concussion.
2. Non-invasive Therapies: Low-Level Laser Therapy (LLLT) and Hyperbaric Oxygen Ketone Therapy (HBOKT)
Non-invasive therapies like Low-Level Laser Therapy (LLLT) and Hyperbaric Oxygen Ketone Therapy (HBOKT) have also been shown to reduce neuroinflammation and promote brain healing. LLLT uses light energy to stimulate cellular repair and reduce inflammation in damaged tissues, while HBOT increases oxygen delivery to the brain, enhancing the brain’s ability to heal and reducing oxidative stress.
Research has demonstrated that both therapies can help alleviate symptoms of PCS by targeting the underlying inflammatory processes that contribute to cognitive decline and mood disorders. These therapies are particularly effective when combined with other interventions, such as nutritional support and cognitive rehabilitation.
3. Lifestyle Changes
In addition to non-invasive therapies and nutritional interventions, lifestyle changes can also play a role in managing neuroinflammation. Regular physical activity has been shown to reduce inflammatory markers and improve cognitive function. Engaging in light aerobic exercise, such as walking or swimming, can promote neuroplasticity and reduce the duration of PCS symptoms. Additionally, stress management techniques, such as meditation and mindfulness, can help regulate the body’s immune response and reduce the production of pro-inflammatory cytokines.
Carolina Brain Center Can Help
At Carolina Brain Center in Raleigh, NC, we understand the importance of managing neuroinflammation to support concussion recovery. Our approach integrates therapies like hyperbaric oxygen ketone therapy, low-level laser therapy, and nutritional interventions to reduce inflammation and promote faster healing. If you’re experiencing prolonged concussion symptoms, don’t wait to seek treatment. By addressing neuroinflammation early, we can help you recover more effectively and prevent long-term complications.
Take the first step toward recovery by filling out our phone consultation request form today. The knowledge and care you receive at Carolina Brain Center will put you on the path to healing.
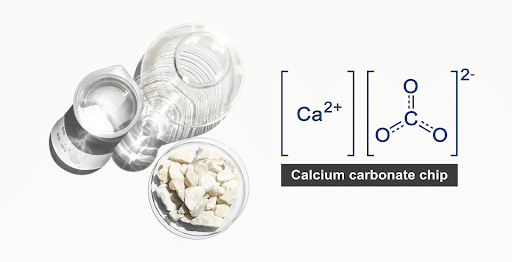
Managing Calcium Dysregulation in Concussion Recovery
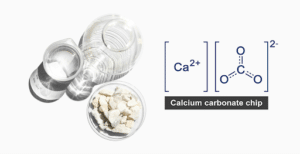
Concussions are often underestimated in terms of the complex biochemical changes they cause within the brain. While immediate symptoms such as headaches and dizziness are more obvious, the underlying cellular disturbances are far more intricate. One of the key processes disrupted after a concussion is calcium homeostasis. Calcium ions (Ca2+) play a critical role in many cellular functions, including signal transmission, muscle contraction, and energy production. However, after a concussion, calcium regulation becomes dysfunctional, contributing to a cascade of problems that can delay recovery and exacerbate symptoms.
Keep reading, as we will begin to explore the impact of calcium dysregulation on brain health following a concussion as well as discuss strategies to manage and mitigate its effects during recovery. By understanding how calcium contributes to both immediate and prolonged symptoms, healthcare professionals and patients can better tailor treatment plans for optimal recovery outcomes.
The Role of Calcium in Neuronal Function
Calcium is essential for neuronal function and signaling. It acts as a messenger that helps transmit signals between neurons by facilitating the release of neurotransmitters across synapses. Calcium also plays a vital role in maintaining the balance of excitatory and inhibitory signals in the brain, helping regulate brain activity. Under normal conditions, neurons tightly regulate calcium levels to ensure proper functioning. Mitochondria and the endoplasmic reticulum act as reservoirs for calcium, releasing it when needed and sequestering it when its levels become too high.
However, when a concussion occurs, the mechanical impact disrupts the cell membranes and leads to a massive influx of calcium into neurons. This excess calcium can overwhelm the cells, triggering a chain reaction that impairs cellular processes, damages mitochondria, and disrupts energy production. The result is an energy crisis in the brain, which contributes to the neurometabolic cascade of concussion.
Calcium Dysregulation and the Neurometabolic Cascade
The neurometabolic cascade that follows a concussion is a series of biochemical reactions that disrupt normal brain function. One of the central components of this cascade is calcium dysregulation. After a concussion, neurons experience a surge in calcium influx, which impairs their ability to function properly. Excess calcium in the cells activates harmful enzymes, such as calpains, which break down proteins and other cellular components, leading to cell death.
This influx of calcium also overwhelms the mitochondria, the energy-producing centers of the cells. Mitochondria are responsible for generating ATP (adenosine triphosphate), the energy currency of cells. However, when overloaded with calcium, mitochondria become dysfunctional and unable to produce sufficient ATP. This contributes to the brain’s energy crisis following a concussion, further impairing cognitive function and prolonging symptoms.
Moreover, calcium dysregulation can trigger oxidative stress, a condition where harmful reactive oxygen species (ROS) are produced in excessive amounts. These ROS cause damage to cellular structures, including membranes, proteins, and DNA. The combination of oxidative stress and impaired energy production creates an environment where the brain cannot heal effectively, leading to persistent symptoms such as headaches, cognitive impairments, and mood disturbances.
The Long-Term Impact of Calcium Dysregulation
If calcium dysregulation is not addressed early in the concussion recovery process, it can lead to long-term consequences. Persistent calcium overload in neurons has been linked to the development of neurodegenerative disorders, such as Alzheimer’s and Parkinson’s disease. Research has shown that chronic calcium dysregulation contributes to the buildup of toxic proteins, such as beta-amyloid, which are associated with neurodegenerative conditions.
Additionally, prolonged calcium imbalances can disrupt the brain’s ability to form new connections, a process known as synaptic plasticity. Synaptic plasticity is critical for learning, memory, and cognitive flexibility. Without proper calcium regulation, the brain becomes less capable of adapting and recovering from the initial injury. This is one reason why some patients experience Post-Concussion Syndrome (PCS), where symptoms such as memory problems, concentration difficulties, and mood disorders persist for months or even years after the initial concussion.
Strategies to Manage Calcium Dysregulation in Concussion Recovery
Given the critical role that calcium plays in both the acute and long-term phases of concussion recovery, managing calcium dysregulation is essential for improving outcomes. Several strategies have emerged that focus on restoring calcium balance and protecting neurons from the damaging effects of calcium overload.
1. Magnesium Supplementation
Magnesium is a natural antagonist to calcium and plays a crucial role in maintaining calcium balance within neurons. After a concussion, magnesium levels often drop, which exacerbates calcium dysregulation. Supplementing with magnesium can help restore this balance by preventing excessive calcium influx and supporting mitochondrial function.
Research has shown that magnesium supplementation can reduce the severity of concussion symptoms and improve recovery outcomes. By stabilizing calcium levels, magnesium helps protect neurons from damage and supports the brain’s ability to generate energy. In addition to magnesium supplementation, maintaining adequate hydration is important, as dehydration can exacerbate electrolyte imbalances, including calcium dysregulation.
2. Mitochondrial Support
Since calcium dysregulation primarily affects mitochondria, supporting mitochondrial function is a key strategy for managing calcium imbalances. Nutritional interventions can help protect mitochondria from oxidative damage and improve their ability to produce ATP. These supplements act as antioxidants, neutralizing reactive oxygen species and reducing oxidative stress.
Hyperbaric oxygen ketone therapy (HBOKT) is another approach that has been shown to enhance mitochondrial function by increasing oxygen delivery to damaged brain tissues. HBOKT can improve energy production and reduce the effects of calcium dysregulation by supporting cellular repair mechanisms. Research suggests that combining HBOKT with other treatments, such as nutritional support and light therapy, may offer synergistic benefits in concussion recovery.
3. Low-Level Laser Therapy (LLLT)
Low-Level Laser Therapy (LLLT) has shown promise in addressing calcium dysregulation by stimulating cellular repair and reducing inflammation. LLLT uses light energy to penetrate the scalp and reach brain cells, where it interacts with mitochondria to enhance ATP production and improve calcium homeostasis. Studies have found that LLLT can reduce oxidative stress and inflammation, both of which are exacerbated by calcium overload in the brain.
By improving mitochondrial function and reducing calcium imbalances, LLLT can help accelerate recovery and alleviate symptoms such as headaches, cognitive impairments, and mood disturbances. This non-invasive therapy is particularly useful for patients with persistent symptoms of Post-Concussion Syndrome.
The Importance of Early Intervention
Calcium dysregulation begins immediately after a concussion, making early intervention critical to preventing long-term damage. The sooner that therapies targeting calcium balance are implemented, the greater the chances of preventing prolonged symptoms and cognitive decline. For patients with a history of multiple concussions or those who experience persistent symptoms, proactive management of calcium dysregulation is especially important for preventing chronic neurological issues.
Healthcare providers should assess calcium regulation as part of the initial evaluation following a concussion and implement strategic support. Early intervention can make a significant difference in the recovery trajectory, reducing the risk of long-term complications and improving overall brain health.
How We Can Help
At Carolina Brain Center, we understand the importance of managing calcium dysregulation in patients recovering from concussions. Our approach integrates innovative therapies such as hyperbaric oxygen therapy, low-level laser therapy, and nutritional interventions to restore calcium balance and support mitochondrial function. By addressing calcium dysregulation early, we help patients recover more quickly and prevent long-term complications.
If you've recently experienced a concussion, don't wait to seek treatment. Early intervention is key to preventing prolonged symptoms and ensuring a full recovery. Take the first step by filling out our phone consultation request form today. The knowledge and care you receive at Carolina Brain Center will set you on the path to healing.
Dealing With Concussions as a Young Adult
 Concussions are a serious issue, especially for young adults. At Carolina Brain Center, we see firsthand how important it is to take brain health seriously, especially when it comes to concussions. In this article, we’ll dive into what concussions are, the differences between getting a concussion as a child versus as a young adult, and why it’s so important to focus on brain health.
Concussions are a serious issue, especially for young adults. At Carolina Brain Center, we see firsthand how important it is to take brain health seriously, especially when it comes to concussions. In this article, we’ll dive into what concussions are, the differences between getting a concussion as a child versus as a young adult, and why it’s so important to focus on brain health.
Understanding Concussions
A concussion is a type of brain injury caused by a bump, blow, or jolt to the head. This sudden movement can make the brain bounce around or twist in the skull, creating chemical changes and sometimes damaging brain cells. Concussions can affect memory, judgment, reflexes, speech, balance, and coordination. The symptoms might show up right after the injury or not until days later. Common signs include headaches, confusion, dizziness, nausea, and sometimes loss of consciousness.
Concussions can happen to anyone at any time. Whether you’re playing sports, involved in a car accident, or even just taking a hard fall, the risk is there. The brain is a sensitive organ, and even a seemingly minor hit can have significant consequences. This is why it’s crucial to recognize the signs and symptoms of a concussion and take immediate action if you suspect you have one.
Concussions in Children vs. Young Adults
Children:
When children get concussions, their brains are still developing. This means they might recover more quickly in some cases, but they also face unique risks. Their brain tissues are more pliable, which can sometimes result in less immediate damage but can cause more long-term issues. Children might have trouble explaining how they feel, making it harder for parents and doctors to understand the severity of the injury. It's also essential to consider their academic and social development. Missing school and activities due to concussion symptoms can significantly impact their growth and learning.
Additionally, children’s brains are more susceptible to the effects of a second concussion if they haven’t fully recovered from the first one. This condition, known as second impact syndrome, can lead to severe complications, including brain swelling and even death. Therefore, it’s crucial for parents and caregivers to ensure children fully recover before returning to any activities that might put them at risk for another head injury.
Young Adults:
For young adults, the situation is different. While their brains have mostly developed, they are more likely to experience lasting effects from concussions. This age group is often involved in high-risk activities like sports, driving, and physically demanding jobs. The pressure to perform academically and socially can also lead to pushing through symptoms rather than resting, which is crucial for recovery. Additionally, young adults are at a stage where they’re making significant life decisions, and a concussion can disrupt plans, career paths, and overall life goals.
Young adults may also face challenges in recognizing the severity of their injury. There’s a tendency to downplay symptoms or attribute them to other causes like stress or lack of sleep. This can delay seeking proper treatment and prolong recovery. Moreover, the demands of higher education or early career responsibilities can make it difficult to take the necessary time off for proper healing.
The Importance of Focusing on Brain Health
Brain health is crucial at any age, but young adults need to pay special attention. Here’s why:
- Academic Performance: Young adults are often in college or starting their careers. A concussion can disrupt studies, lead to missed classes, and lower grades. It's important to recognize that rest and recovery are essential to getting back on track.
Academic pressure can be intense, and trying to keep up with coursework while dealing with concussion symptoms can be overwhelming. It’s essential to communicate with professors and academic advisors about your condition. Many educational institutions have accommodations in place for students recovering from concussions, such as extended deadlines and adjusted workloads. - Long-term Impact: Ignoring concussion symptoms can lead to long-term problems. Chronic headaches, memory issues, and mood changes can significantly affect one's quality of life. It’s vital to address concussions properly to avoid these long-term consequences.
Long-term impacts aren’t just physical. Persistent concussion symptoms can lead to feelings of frustration, anxiety, and depression. It’s important to seek support not only for the physical aspects of recovery but also for the emotional and psychological challenges that may arise. - Mental Health: Concussions can lead to anxiety, depression, and other mental health issues. Young adults already face significant stress from their responsibilities, and a concussion can exacerbate these problems.
Mental health is just as important as physical health. If you’re experiencing mood changes, difficulty sleeping, or feelings of sadness or anxiety following a concussion, don’t hesitate to seek help from a mental health professional. Addressing these issues early can prevent them from becoming more severe over time. - Holistic Healthcare: At Carolina Brain Center, we emphasize the importance of holistic healthcare services. Treating a concussion isn’t just about addressing the immediate symptoms but also about supporting overall health. This includes physical therapy, nutritional counseling, and stress management.
Holistic care involves looking at the whole person, not just the injury. By supporting the body’s natural healing processes and addressing all aspects of health, we can help you recover more fully and prevent future issues. This approach can include chiropractic care, massage therapy, acupuncture, and other complementary treatments that support the body’s healing.
How to Handle a Concussion
If you suspect you have a concussion, here’s what to do:
- Seek Medical Attention: Visit a healthcare professional who specializes in concussions. If you're in the area, consider a visit to a concussion clinic in Raleigh, NC. They can perform a thorough evaluation and recommend the best course of treatment.
- Rest and Recovery: Give your brain time to heal. Avoid physical activities and get plenty of sleep. It might be frustrating, but it's crucial for recovery.
Rest doesn’t just mean avoiding physical exertion. It also means giving your brain a break from cognitive activities that can strain it, such as reading, screen time, and problem-solving tasks. Take it easy and allow yourself the time to heal. - Follow Up: Keep up with follow-up appointments to monitor your progress. Sometimes symptoms can change or new ones can appear later on.
Regular check-ins with your healthcare provider can help ensure you’re on the right track and allow for adjustments to your treatment plan as needed. Don’t skip these appointments, even if you’re feeling better. - Holistic Approach: Look into holistic healthcare services to support your recovery. At Carolina Brain Center, we offer a range of services to help with concussion recovery, from chiropractic care to nutritional advice.
Incorporating holistic treatments can enhance your recovery process. Nutritional counseling, for example, can ensure you’re getting the nutrients needed to support brain health and healing. Stress management techniques like mindfulness and relaxation exercises can help reduce stress and promote overall well-being.
Why Choose a Chiropractic Neurologist?
Dealing with a concussion is not just about immediate treatment; it’s about long-term care. Visiting a neurologist specializing in post concussion syndrome can make a significant difference. Specialists understand the complexities of brain injuries and can provide personalized care plans. They can help manage symptoms, offer rehabilitation options, and provide support for mental health issues that might arise.
Choosing a specialist means you’re getting care from someone who has extensive experience and knowledge in treating concussions and their aftermath. They can offer advanced diagnostic tools and treatment options that general practitioners might not have access to.
Prevention Tips
Preventing concussions is as important as treating them. Here are some tips:
- Wear Protective Gear: Whether you're playing sports or working in a risky environment, always wear appropriate protective gear.
Helmets, pads, and other protective equipment are designed to absorb impact and reduce the risk of injury. Make sure your gear fits properly and is in good condition. - Follow Safety Guidelines: Adhere to safety rules in sports, driving, and other activities.
Safety rules are there for a reason. Following them can significantly reduce your risk of injury. Be aware of your surroundings and take precautions to protect yourself. - Educate Yourself: Learn about the symptoms of concussions and take them seriously. Educate friends and family, too, so they understand the importance of brain health.
The more you know about concussions, the better prepared you’ll be to recognize and respond to them. Share this knowledge with others to help create a safer environment for everyone. - Stay Fit: Physical fitness can help improve balance and coordination, reducing the risk of falls and injuries.
Regular exercise strengthens your muscles and improves your balance, making you less likely to fall or sustain an injury. Activities like yoga and tai chi can be particularly beneficial for enhancing balance and coordination.
The Role of Carolina Brain Center
At Carolina Brain Center, we are committed to helping young adults navigate the challenges of concussions. Our team offers comprehensive care tailored to each individual. We believe in treating the whole person, not just the symptoms. From initial assessment to long-term recovery plans, we are here to support you every step of the way.
Concussions are a serious issue, especially for young adults. Understanding the differences between concussions in children and young adults, focusing on brain health, and seeking proper care are all crucial steps in dealing with this injury. If you or someone you know is dealing with a concussion, don't hesitate to reach out to a concussion clinic in Raleigh, NC, or find a neurologist specializing in post concussion syndrome near me. Remember, taking care of your brain is taking care of your future.
For more information or to schedule an appointment with chiropractic neurologist Dr. Dane, please head to CarolinaBrainCenter.com. We're here to help you on your journey to recovery and overall brain health.
Using the Erchonia Laser to Help Manage Pain
 When it comes to managing pain, especially chronic pain, finding effective treatments can be a challenge. At Carolina Brain Center, we pride ourselves on offering innovative and holistic healthcare services to help our patients live healthier, more comfortable lives. One of the standout treatments we offer is the Erchonia Laser, a powerful tool in managing pain, particularly for those suffering from neurological degenerative disorders and degenerative brain disease. Let's dive into how this amazing technology can help you.
When it comes to managing pain, especially chronic pain, finding effective treatments can be a challenge. At Carolina Brain Center, we pride ourselves on offering innovative and holistic healthcare services to help our patients live healthier, more comfortable lives. One of the standout treatments we offer is the Erchonia Laser, a powerful tool in managing pain, particularly for those suffering from neurological degenerative disorders and degenerative brain disease. Let's dive into how this amazing technology can help you.
What is the Erchonia Laser?
The Erchonia Laser is a type of low-level laser therapy (LLLT) that uses specific wavelengths of light to interact with tissue. This interaction promotes healing and alleviates pain. Unlike high-intensity lasers that cut or burn tissue, the Erchonia Laser is non-invasive and painless. It works at a cellular level to reduce inflammation, promote cell regeneration, and enhance blood flow. This is crucial for patients dealing with conditions like neurological degenerative disorders and degenerative brain disease, where managing pain and promoting healing are top priorities.
How Does the Erchonia Laser Work?
The magic of the Erchonia Laser lies in its ability to stimulate the body's natural healing processes. When the laser light penetrates the skin, it triggers a series of events in the cells:
- Increased ATP Production: The laser light stimulates the mitochondria in cells to produce more ATP (adenosine triphosphate), which is the energy currency of cells. This boost in energy helps cells repair and regenerate faster.
- Reduced Inflammation: The laser light reduces the production of pro-inflammatory cytokines and increases the production of anti-inflammatory cytokines. This shift helps decrease inflammation and pain.
- Enhanced Blood Flow: The laser stimulates the formation of new blood vessels and improves circulation. Better blood flow means more oxygen and nutrients are delivered to the tissues, promoting faster healing.
- Pain Reduction: The Erchonia Laser modulates nerve function, helping to reduce the transmission of pain signals to the brain.
Benefits of Erchonia Laser for Neurological Degenerative Disorders
Patients with neurological degenerative disorders, such as Alzheimer's disease, Parkinson's disease, and multiple sclerosis, often experience significant pain and discomfort. Traditional pain management strategies can be limited and may come with unwanted side effects. The Erchonia Laser offers a safe and effective alternative with several benefits:
- Non-Invasive and Painless: Patients do not need to worry about the discomfort associated with needles, incisions, or heat. The treatment is entirely non-invasive.
- No Side Effects: Unlike medications, which can cause various side effects, the Erchonia Laser has no known adverse effects.
- Promotes Healing: Beyond just managing pain, the laser helps in healing the tissues, potentially slowing down the progression of degenerative conditions.
Combining Erchonia Laser with Chiropractic Care
At Carolina Brain Center, we believe in a comprehensive approach to healthcare. Combining the Erchonia Laser with traditional chiropractic care can amplify the benefits for our patients.
- Spinal Adjustments: Chiropractic adjustments help realign the spine, improving nervous system function. When combined with the Erchonia Laser, these adjustments can be even more effective, as the laser enhances the healing of tissues and reduces inflammation around the spine.
- Holistic Healthcare Services: Our holistic approach means we look at the whole person, not just the symptoms. By integrating the Erchonia Laser into a broader treatment plan that includes nutrition, exercise, and lifestyle changes, we can address the root causes of pain and discomfort.
Real-Life Success Stories
We've seen firsthand how the Erchonia Laser has transformed the lives of our patients. For instance, one patient with Parkinson's disease experienced a significant reduction in muscle stiffness and pain after several sessions. Another patient with chronic migraines found relief that they hadn't experienced with other treatments. These stories are a testament to the power of combining advanced technology with holistic healthcare services.
What to Expect During Treatment
If you're considering Erchonia Laser therapy, here's what you can expect:
- Initial Consultation: We'll start with a thorough consultation to understand your medical history, current health status, and specific pain points. This helps us tailor the treatment to your needs.
- Customized Treatment Plan: Based on the consultation, we'll create a personalized treatment plan. This may include a combination of Erchonia Laser sessions and chiropractic adjustments.
- Laser Sessions: During a laser session, you'll sit or lie comfortably while the laser is applied to the targeted area. The sessions are quick, usually lasting around 10-20 minutes.
- Follow-Up and Progress Monitoring: We'll schedule follow-up appointments to monitor your progress and make any necessary adjustments to your treatment plan.
FAQs About Erchonia Laser Therapy
Q: Is Erchonia Laser therapy safe?
A: Yes, Erchonia Laser therapy is FDA-approved and has been shown to be safe for various conditions. It's non-invasive and has no known side effects.
Q: How many sessions will I need?
A: The number of sessions varies depending on the condition and the patient's response to treatment. Typically, patients start to see improvements after just a few sessions.
Q: Does the treatment hurt?
A: No, the treatment is painless. Patients may feel a slight warming sensation, but it is generally very comfortable.
Q: Can it be used for other conditions?
A: Yes, Erchonia Laser therapy is versatile and can be used for a variety of conditions, including sports injuries, arthritis, and post-surgical recovery.
Taking the Next Step Towards Pain Relief
If you're struggling with pain from neurological degenerative disorders or degenerative brain disease, the Erchonia Laser could be the solution you've been looking for. At Carolina Brain Center, we're committed to providing holistic healthcare services that address both the symptoms and the root causes of your pain. Combining cutting-edge technology like the Erchonia Laser with traditional chiropractic care allows us to offer comprehensive and effective treatment plans.
Ready to experience the benefits of Erchonia Laser therapy? Contact Dr. Dane today to schedule your consultation and take the first step towards a pain-free life. Let us help you get back to doing the things you love, free from the burden of chronic pain.
7 Tips to Improve Brain Health in Your 30’s
 Hey there! If you're in your 30s, it's a great time to start thinking about your brain health. You might be focused on your career, family, or just enjoying life, but taking care of your brain now can pay off big time down the road. This is especially true if you have a family history of neurological degenerative disorders like dementia or Alzheimer's. Don't worry, though—taking care of your brain can be simple and even fun! Here are seven tips to help you keep your brain in tip-top shape.
Hey there! If you're in your 30s, it's a great time to start thinking about your brain health. You might be focused on your career, family, or just enjoying life, but taking care of your brain now can pay off big time down the road. This is especially true if you have a family history of neurological degenerative disorders like dementia or Alzheimer's. Don't worry, though—taking care of your brain can be simple and even fun! Here are seven tips to help you keep your brain in tip-top shape.
1. Stay Active
Exercise isn't just great for your body; it's awesome for your brain too! Regular physical activity increases blood flow to your brain, which can help keep it healthy and strong. Aim for at least 30 minutes of moderate exercise most days of the week. This can be anything from a brisk walk, a fun dance class, or even playing a sport you love.
Why it matters: Exercise has been shown to improve memory and thinking skills. It's a natural way to boost your brain's health and keep neurological degenerative disorders at bay.
Tips for staying active: Find an activity you enjoy so that it doesn't feel like a chore. Whether it's hiking, cycling, or even gardening, as long as you're moving, your brain will benefit. Try to mix up your routine to keep things interesting and challenge different parts of your brain and body.
2. Eat Brain-Boosting Foods
What you eat has a big impact on your brain health. Focus on a diet that's rich in fruits, vegetables, whole grains, and lean proteins. Omega-3 fatty acids, found in fish like salmon and nuts like walnuts, are especially good for your brain.
Why it matters: A healthy diet can help reduce inflammation and provide the nutrients your brain needs to function properly. It's one of the best holistic healthcare services you can give yourself!
Brain-boosting foods to include: Blueberries, turmeric, broccoli, pumpkin seeds, and dark chocolate. These foods are packed with antioxidants, vitamins, and minerals that support brain health. Try to incorporate a variety of these foods into your meals to get the full range of benefits.
3. Get Enough Sleep
Sleep is crucial for your brain. When you sleep, your brain has a chance to repair itself and clear out toxins that can lead to degenerative brain disease. Aim for 7-9 hours of quality sleep each night.
Why it matters: Consistent, quality sleep can improve memory, mood, and overall cognitive function. It's like hitting the reset button for your brain every night.
Tips for better sleep: Establish a regular sleep schedule by going to bed and waking up at the same time every day. Create a relaxing bedtime routine, such as reading a book or taking a warm bath. Make your sleep environment comfortable and free from distractions, like electronics and excessive noise.
4. Challenge Your Mind
Keeping your brain active is just as important as keeping your body active. Engage in activities that challenge your brain, such as puzzles, reading, learning a new skill, or playing an instrument.
Why it matters: Mental stimulation strengthens the connections between your brain cells and can even create new ones. It's a fun way to keep your brain sharp and fend off neurological degenerative disorders.
Ways to challenge your mind: Take up a new hobby that interests you, such as painting, knitting, or coding. Join a book club or take an online course in a subject you've always wanted to learn about. The key is to keep your mind engaged and continuously learning.
5. Stay Social
Spending time with friends and family isn't just fun—it’s great for your brain too! Social interactions can help improve your mood and cognitive function.
Why it matters: Strong social connections can lower the risk of degenerative brain disease. So go ahead, plan that game night or coffee date—it’s good for your brain!
Tips for staying social: Make an effort to reach out to friends and family regularly, even if it's just a quick phone call or text message. Join social groups or clubs that align with your interests. Volunteering is another excellent way to meet new people and stay socially active.
6. Manage Stress
Chronic stress can take a toll on your brain health. Finding ways to manage stress, whether through meditation, yoga, or just taking time to relax, can help keep your brain healthy.
Why it matters: Reducing stress can improve brain function and lower the risk of neurological degenerative disorders. It's an essential part of holistic healthcare services.
Stress management techniques: Practice mindfulness meditation or deep breathing exercises to help calm your mind. Engage in activities that you find relaxing, such as listening to music, spending time in nature, or practicing a hobby. Remember to take breaks throughout the day to avoid burnout.
7. Avoid Harmful Habits
Things like smoking and excessive drinking can have a negative impact on your brain health. Try to avoid these habits and replace them with healthier ones.
Why it matters: Avoiding harmful habits can protect your brain from damage and reduce the risk of degenerative brain disease. It's never too late to make a positive change!
Healthier habits to adopt: If you smoke, consider seeking help to quit, such as joining a support group or using nicotine replacement therapies. Limit your alcohol intake to moderate levels, which is generally one drink per day for women and two for men. Focus on building healthy routines, such as regular exercise, a balanced diet, and adequate sleep.
It’s Time Take Care of Your Brain
Taking care of your brain in your 30s is a smart move, especially if you have a family history of neurological degenerative disorders. By staying active, eating well, getting enough sleep, challenging your mind, staying social, managing stress, and avoiding harmful habits, you can keep your brain healthy and strong. Remember, it's the small, everyday actions that add up to make a big difference. Start today and give your brain the best chance for a healthy future! Contact Carolina Brain Center today, to learn more.
FAQs About Taking Care of Your Brain in Your 30’s
Q: What are neurological degenerative disorders?
A: These are conditions that cause the brain to deteriorate over time, such as Alzheimer's and dementia.
Q: Can diet really affect brain health?
A: Yes! Eating a balanced diet rich in brain-boosting foods can help keep your brain healthy.
Q: How does exercise benefit the brain?
A: Exercise increases blood flow to the brain, which can improve memory and cognitive function.
Q: Why is sleep so important for brain health?
A: Sleep helps the brain repair itself and clear out toxins, which is crucial for maintaining cognitive function.
Q: What are some good brain-challenging activities?
A: Puzzles, reading, learning a new skill, and playing an instrument are all great ways to challenge your brain.
Q: How can I manage stress to improve brain health?
A: Techniques like meditation, yoga, and taking time to relax can help reduce stress and improve brain function.
Q: Why should I avoid smoking and excessive drinking?
A: These habits can damage your brain and increase the risk of degenerative brain diseases.
By following these tips, you can help ensure your brain stays healthy and strong for years to come. Your 30s are a great time to start focusing on brain health, so take action today and give your brain the care it deserves!
Why Caring for Your Brain Now is Key to Your Future Success

If you're in your 20s or 30s, you're probably juggling a million things: starting a career, maybe continuing your education, and trying to maintain a social life. Amid all this hustle, it's easy to overlook something as crucial as brain health. But here's the thing – taking care of your brain now can give you that extra edge in school, boost your career, and keep you sharp for years to come. At Carolina Brain Center, we offer a range of wellness plans designed to help you keep your brain in top shape. Let's dive into why brain health matters and how you can start taking care of it today.
The Importance of Brain Health in Your 20s and 30s
Your 20s and 30s are critical years for brain development and health. This period sets the foundation for your cognitive abilities later in life. Habits and practices you adopt now can either protect your brain from neurological degenerative disorders or increase your risk of developing them. Here are some reasons why focusing on brain health now is so important:
- Maximize Cognitive Function: Your brain is still developing and refining its neural connections. Keeping it healthy can enhance your memory, learning capabilities, and problem-solving skills.
- Prevent Neurological Disorders: Early prevention can significantly reduce the risk of neurological degenerative disorders like Alzheimer's and Parkinson's later in life.
- Boost Academic and Career Performance: A healthy brain can improve your focus, productivity, and creativity, giving you a competitive edge in your studies or career.
Wellness Plans at Carolina Brain Center
At Carolina Brain Center, we understand the unique needs of young adults and offer a variety of wellness plans to help you maintain optimal brain health. Here's what we provide:
- Yearly Baseline Neurological Exams: These exams help us track your brain health over time and identify any potential issues early on.
- Neurocognitive Testing: Done privately at home, these tests can assess your cognitive functions like memory, attention, and processing speed.
- Hyperbaric Oxygen Ketone Therapy (HBOKT): This therapy increases oxygen delivery to the brain, promoting healing and improving cognitive functions.
- GyroStim: A cutting-edge tool that stimulates your vestibular system to enhance balance, coordination, and cognitive function.
- Nutritional Counseling: Proper nutrition is vital for brain health. Our experts can help you develop a diet that supports your cognitive functions.
- Erchonia Low-Level Laser Therapy (LLLT): This non-invasive therapy can help reduce inflammation and promote brain healing.
- Individualized Brain Games and Activities: Tailored to your needs, these activities are designed to keep your brain engaged and improve various cognitive functions.
- Chiropractic Care: Regular adjustments can improve your overall health and well-being, including brain function.
Practical Steps to Boost Your Brain Health
Now that you know the importance of brain health and the services we offer, here are some practical steps you can take to keep your brain in top shape:
- Stay Active: Regular physical exercise increases blood flow to the brain and promotes the growth of new brain cells. Aim for at least 30 minutes of moderate exercise most days of the week.
- Eat Brain-Healthy Foods: Incorporate foods rich in omega-3 fatty acids, antioxidants, and vitamins. Think salmon, blueberries, nuts, and leafy greens.
- Get Enough Sleep: Quality sleep is crucial for memory consolidation and overall brain function. Aim for 7-9 hours of sleep per night.
- Manage Stress: Chronic stress can negatively impact your brain health. Practice stress-reducing techniques like meditation, yoga, or deep breathing exercises.
- Stay Mentally Active: Engage in activities that challenge your brain, such as puzzles, reading, or learning a new skill.
- Stay Socially Connected: Social interactions can help keep your brain active and reduce the risk of cognitive decline.
Why Choose Carolina Brain Center?
You might be wondering why you should choose Carolina Brain Center for your brain health needs. Here are a few reasons:
- Expertise in Neurological Care: Our team includes highly trained neurological chiropractors who specialize in brain health.
- Comprehensive Wellness Plans: We offer a holistic approach to brain health, covering everything from exams and therapies to nutrition and cognitive activities.
- Personalized Care: We understand that each person is unique, and we tailor our services to meet your specific needs and goals.
- Convenience and Comfort: Many of our services, like neurocognitive testing, can be done from the comfort of your home.
Invest In Your Future
Taking care of your brain now is one of the best investments you can make in your future. Whether you're looking to excel in school, advance in your career, or simply maintain your cognitive health, the steps you take today can have a profound impact. At Carolina Brain Center, we're here to support you every step of the way with our comprehensive wellness plans and expert care. Don't wait – start prioritizing your brain health today!
Remember, your brain is your most valuable asset. Treat it with the care and attention it deserves, and it will serve you well for years to come. If you're ready to take the next step in your brain health journey, contact Dr. Dane at Carolina Brain Center and let us help you achieve your goals.
By focusing on brain health now, you're not just preparing for a brighter future – you're enhancing your present. With the right support and guidance, you can unlock your brain's full potential and enjoy the benefits in every aspect of your life. So, what are you waiting for? Let's get started on this exciting journey together!
Feel free to reach out to Carolina Brain Center to learn more about our wellness plans and how we can help you achieve optimal brain health. Your future self will thank you!