Understanding the Vestibular System: Symptoms, Impact, and Treatment
Understanding the Vestibular System: Symptoms, Impact, and Treatment

When we consider the vestibular system, we typically visualize the inner ear and associate it with symptoms such as dizziness and vertigo. However, the vestibular system is much more than that; it is a complex and extensive sensory network. This crucial system is essential for maintaining balance, spatial awareness, and coordination of movement, but its impact extends beyond the physical realm. It plays a significant role in cognitive function, emotional regulation, and has a profound effect on the autonomic nervous system. Understanding the vestibular system's comprehensive role can help us appreciate its importance in overall health and well-being.
Vestibular Dysfunction Symptoms
Vestibular dysfunction can manifest in a variety of symptoms, which may vary significantly in their impact on daily life. Common symptoms include:
- Dizziness: A broad term that describes a range of sensations, including lightheadedness and a feeling of unsteadiness.
- Vertigo: A specific type of dizziness characterized by the sensation that you or your surroundings are spinning or moving.
- Motion sickness: Discomfort experienced during movement, often due to conflicting sensory signals.
- Environmental motion intolerance: Difficulty tolerating visual or physical stimuli, such as busy environments or rapid head movements.
- Blurred or double vision: Visual disturbances linked to imbalance in coordination.
- Headaches and neck pain: Often associated with muscle tension or strain due to compensatory behaviors.
- Nausea and vomiting: Common visceral responses to vestibular disturbances.
- Clumsiness or difficulty coordinating movements: Resulting from impaired balance mechanisms.
- Difficulty focusing and impaired spatial awareness: Challenges in understanding one’s position in space can impact activities like reading or driving.
- Emotional symptoms: Anxiety, depression, and mood swings are frequently reported and can be exacerbated by the disorientation and uncertainty of vestibular dysfunction.
The vestibular system begins developing around 7 weeks after conception, establishing a foundation for balance and motor coordination. Utilizing specialized organs like the utricle and saccule, this system detects gravitational forces. It also relies on the semicircular canals to sense rotational movements.
The extensive impact of vestibular disorders on cognitive clarity, emotional regulation, and overall well-being cannot be overstated. Ineffective balance can hinder one’s ability to perceive social cues and navigate environments effectively, leading to confusion and potential learning challenges. Balance issues can also deplete cognitive resources, further complicating learning and memory.
From an emotional standpoint, disruptions in vestibular function can contribute to heightened anxiety levels and mood instability. Chronic vestibular conditions can lead to social withdrawal, panic attacks, or specific phobias, underscoring the psychological dimensions of these disorders. Additionally, persistent dysfunction may impair higher-order cognitive functions essential for problem-solving and decision-making.
In summary, the vestibular system is vital to our sensory and motor integration, influencing numerous daily life aspects. Given its critical role, vestibular dysfunction should not be overlooked or under-treated; increased awareness and timely intervention are crucial for those affected.
Contact Us
At Carolina Brain Center, in Raleigh, NC, we understand the importance of addressing vestibular dysfunction, as it affects 90% of our patient population. Unfortunately, this vital system is often overlooked and under-treated by many practitioners. That’s why we meticulously assess the vestibular system in all new patients—it's often a crucial factor in achieving successful treatment outcomes.
If you are experiencing symptoms related to concussions, traumatic brain injuries (TBI), strokes, Parkinson’s disease, anxiety disorders, chronic pain syndromes, headaches, or if you identify as one of our "dizzy" patients, we want to help you. Even if you’ve received treatment elsewhere and are still struggling, don’t lose hope!
Complete our consultation request form today, and Dr. Dane will personally reach out to discuss your symptoms. This initial phone call is complimentary—so take the first step towards a healthier you!
Is the Neurometabolic Cascade of Your Concussion Being Addressed by Your Concussion Specialist?

The neurometabolic cascade of concussion (NMCC) refers to the complex biochemical processes that occur following a concussion and can lead to significant brain energy deficits and prolonged recovery from a concussion when not adequately addressed. Prioritizing the treatment of the neurometabolic cascade of concussion (NMCC) is a key factor in Dr. Dane's remarkable success with patients suffering from both acute concussions and post-concussion syndrome. Dr. Dane is deeply committed to addressing this often under-treated aspect of concussion management. Recognizing its importance, she will conduct a training session for her colleagues in October 2024, where she will share her expertise on the NMCC and effective treatment strategies. As a trailblazer in her field, Dr. Dane's colleagues consistently value her insights as she seamlessly integrates cutting-edge medical research into everyday patient care—resulting in outstanding outcomes.
The Neurometabolic Cascade of Concussion
In 2001, Giza and Hovda defined the NMCC and then expanded their research in 2014. Since then, over 400 other research articles have cited this landmark information.
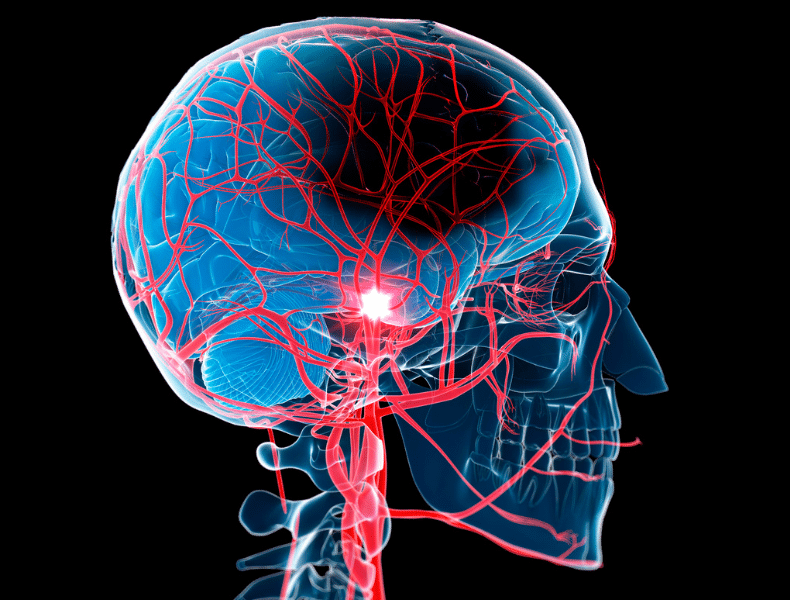
The cascade starts immediately following the biomechanical injury which includes the impact and neuronal stretching. The main issue that results from the NMCC is an energy crisis in the brain. This means the energy demand is greater than energy production. What causes the energy crisis is multifactorial and described in detail by the NMCC. The goal of this article is to highlight and summarize the main causes associated with the NMCC: (1) increased glutamate, (2) a massive efflux of potassium, and (3) poor mitochondrial function. It is also essential to understand that the NMCC is happening in the presence of decreased cerebral blood flow, which further contributes to the energy crisis.
Increased Glutamate Levels
A concussion’s impact leads to increased release of an excitatory amino acid called glutamate. Glutamate hinders cellular transport of glucose into cells, where the mitochondria can turn glucose into ATP (adenosine triphosphate) the fuel substrate for all cells. High glutamate levels also promote the efflux of potassium out of the cells, which leads to excitotoxicity and is associated with noise and light sensitivity and irritability.
Potassium Efflux
The sodium-potassium (Na-K) pump is essential for regulating cellular homeostasis. The pump runs on ATP. ATP, or adenosine triphosphate, is the energy currency of cells. When there is a massive efflux (moving out of the cell) of potassium, the Na-K pump's demand for ATP increases to get the potassium back in the cell. This creates a high demand for glucose so that ATP can be produced in higher quantities. At this point, there is an increase in glycolysis, which leads to lactate accumulation.
Mitochondrial Dysfunction
The increased need for ATP production by the mitochondria is impaired by calcium overload. This leads to poor mitochondrial function and ATP production due to impaired oxidative metabolism. The process by which glucose is turned into ATP is an oxidative process.
Other important components of the NMCC
Lactate accumulation - Elevated lactate levels can impair neuronal function through a series of mechanisms:
- Inducing acidosis
- Causing membrane damage
- Altering blood-brain barrier permeability
- Leading to cerebral edema
- Promoting Amyloid-β protein deposition
Lactylation-associated pathology includes cancer, neuropsychiatric illness, multiple sclerosis, and Alzheimer's disease.
Reductions in Magnesium
Intracellular magnesium levels are also immediately reduced after TBI and remain low for up to 4 days. This reduction has been correlated with post-injury neurologic deficits.
- Both glycolytic and oxidative generation of ATP are impaired when magnesium levels are low.
- Magnesium is necessary for maintaining the cellular membrane potential and initiating protein synthesis.
- Low magnesium levels may effectively unblock the NMDA receptor channel more easily, leading to a greater influx of Ca2+.
Immunoexcitotoxicity
Recent studies suggest that mild TBI triggers inflammatory changes. The studies report extensive upregulation of cytokine and inflammatory genes after TBI.
Microglial activation after adult FPI (fluid percussion injury) has been associated with damage to the substantia nigra and implicated in the increased risk for parkinsonism after TBI.
A theory relating glutamate release and activation of immune receptors to oxidative stress and potentially later cellular injury has been proposed and termed “immunoexcitotoxicity.”
Treating the Neurometabolic Cascade of Concussion
At Carolina Brain Center, Dr. Dane, has developed protocols specifically to address the NMCC. The treatments dampen increased levels of glutamate, increase fuel, improve mitochondrial function, dampen inflammatory responses, and improve cerebral blood flow.
Ketones1,2,3,4,5
Ketone bodies, specifically Beta-Hydroxybutyrate (BHB), can be produced by your own body by following a ketogenic diet or taken exogenously. BHB provides alternative fuel when glucose availability is compromised and have garnered interest for their potential health benefits and applications in concussion and other types of traumatic brain injuries. Studies suggest that administering ketones to TBI patients could significantly aid in their recovery and provide a promising nonpharmacologic treatment for TBI.
- Ketone bodies (KBs) can help address post-traumatic cerebral energy deficits. Exogenous ketone ester supplementation has been shown to be the brain’s preferred energy source, even when glucose is readily available.
- Ketone bodies reduce inflammation, oxidative stress, and neurodegeneration. KBs directly regulate mitochondrial permeability transition, thus affecting the regulation of intracellular calcium levels.
- Ketone bodies limit glutamate release and upregulate GAD1, increasing glutamate conversion to GABA.
- Preliminary evidence suggests that inducing ketosis with exogenous ketones may help improve cognitive and motor performance in conditions such as seizure disorders, mild cognitive impairment, Alzheimer's disease, and neurotrauma.
Transcranial Low-Level Laser Therapy (tLLLT)6,7
The NMCC results in an energy crisis involving mitochondrial function in an environment with reduced cerebral blood flow. Vascular damage causes hypoxia associated with high levels of glycolysis, reduced ATP generation, increased formation of reactive oxygen species (ROS), and apoptosis (cell death).
Light absorption in the electron transport chain of the mitochondria reduces brain damage and supports the brain's natural repair processes after injury by producing a shift in the mitochondria's redox state, leading to the regulation of transcription factors and redox-sensitive genes.
Transcranial low-level laser profoundly and positively affects mitochondrial function, decreases tissue edema and inflammation, decreases excitotoxicity, improves cerebral blood flow, and increases angiogenesis, synaptogenesis, neurotrophins, and neural progenitor cells.
Combining low-level lasers with specific energy sources and substances that influence energy production significantly enhances the therapy's neuroprotective and therapeutic effects. This combined approach holds great promise, particularly in tissues with low energy production, such as the injured brain. It has shown encouraging results in protecting the hippocampal region and restoring cognitive and learning abilities and motor function.
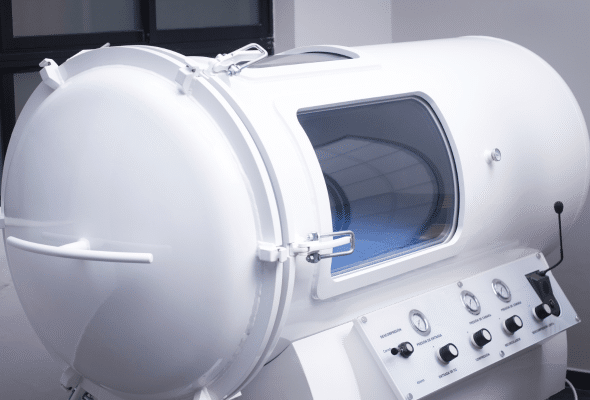
Mild Hyperbaric Oxygen Therapy8,9,10
Hyperbaric oxygen therapy targets TBI-induced ischemia by producing an increased O2 concentration in the plasma and, thus, improved delivery of O2 for diffusion to brain tissue.
Cerebral blood flow is normally regulated by cerebral metabolism. This metabolic coupling is improved by HBOT.
Apoptosis within the hippocampus and general hippocampal neuronal integrity have also been repeatedly shown to benefit from HBO2, potentially through an anti-inflammatory mechanism. Biomarkers, including neutrophil infiltration, TNF-a, IL-1b, IL-6, IL-10, and MCP1, were reduced following HBOT, and subjects had consistently better functional outcomes and reduced lesion volumes.
Additional support for HBOT’s neuroprotective effect after TBI includes findings of reduced blood-brain barrier (BBB) permeability and dysfunction and infarction volume, as well as increased neuronal density, neuronal integrity, neurogenesis, synaptogenesis, and axonal integrity.
Mild hyperbaric oxygen improves oxidative metabolism in cells and tissues without barotrauma and excessive production of reactive oxygen species. Symptom improvement was greatest at 1.3ATM.
Your Concussion Rehabilitation Starts at Carolina Brain Center
After reading all this, you might wonder, “Why has no one ever mentioned this?” The positive takeaway is that you are now more educated about the pathophysiology of concussions and other types of traumatic brain injuries than most people. Knowledge is POWER!
For the person who just had a concussion, many times, you don’t feel well enough to start treatment, and sometimes, all you need is help in calming down the NMCC. If you can lie in bed, you can lie in our extra-large hyperbaric chamber. For the acute patient, we do a combination of hyperbaric oxygen ketone therapy and transcranial low-level laser therapy to start you on the road to recovery. Because many concussions are self-limiting, this may be the only treatment you need!
For the post-concussive patient who is not recovering on their own, we still need to reverse the effects of the NMCC using these same innovative strategies. In addition, we tailor a rehabilitation journey just for you that will be done at home and here in the office. Combination home and office strategies save you time and money. For more complex cases, we offer intensive therapy here at the office before moving to the blended in-office and at-home strategy.
To start the conversation, fill out our phone consultation request form. The call is free but the knowledge is priceless.
References
1 Daines, S. A. (2021). The Therapeutic Potential and Limitations of Ketones in Traumatic Brain Injury. Frontiers in Neurology, 12, 723148. https://doi.org/10.3389/fneur.2021.723148
2 Edwards, M. G., Andersen, J. R., Curtis, D. J., Riberholt, C. G., & Poulsen, I. (2024). Diet-induced ketosis in adult patients with subacute acquired brain injury: A feasibility study. Frontiers in Medicine, 10, 1305888. https://doi.org/10.3389/fmed.2023.1305888
3 Paoli, A., Moro, T., Bosco, G., Bianco, A., Grimaldi, K. A., Camporesi, E., & Mangar, D. (2015). Effects of n-3 polyunsaturated fatty acids (ω-3) supplementation on some cardiovascular risk factors with a ketogenic Mediterranean diet. Marine drugs, 13(2), 996–1009. https://doi.org/10.3390/md13020996
4 Poff, A. M., Moss, S., Soliven, M., & P., D. (2021). Ketone Supplementation: Meeting the Needs of the Brain in an Energy Crisis. Frontiers in Nutrition, 8, 783659. https://doi.org/10.3389/fnut.2021.783659
5 Sethi, S., Wakeham, D., Ketter, T., Hooshmand, F., Bjornstad, J., Richards, B., Westman, E., Krauss, R. M., & Saslow, L. (2024). Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial. Psychiatry Research, 335, 115866. https://doi.org/10.1016/j.psychres.2024.115866
6 Khuman J, Zhang J, Park J, Carroll JD, Donahue C, Whalen MJ. Low-level laser light therapy improves cognitive deficits and inhibits microglial activation after controlled cortical impact in mice. J Neurotrauma 2012;29:408–417
7 Thunshelle, C., & Hamblin, M. R. (2016). Transcranial Low-Level Laser (Light) Therapy for Brain Injury. Photomedicine and Laser Surgery, 34(12), 587-598. https://doi.org/10.1089/pho.2015.4051
8 Daly, S., Thorpe, M., Rockswold, S., Hubbard, M., Bergman, T., Samadani, U., & Rockswold, G. (2018). Hyperbaric Oxygen Therapy in the Treatment of Acute Severe Traumatic Brain Injury: A Systematic Review. Journal of neurotrauma, 35(4), 623–629. https://doi.org/10.1089/neu.2017.5225
9 Harch P. G. (2022). Systematic Review and Dosage Analysis: Hyperbaric Oxygen Therapy Efficacy in Mild Traumatic Brain Injury Persistent Postconcussion Syndrome. Frontiers in neurology, 13, 815056. https://doi.org/10.3389/fneur.2022.815056
10 Ishihara A. (2019). Mild hyperbaric oxygen: mechanisms and effects. The journal of physiological sciences : JPS, 69(4), 573–580. https://doi.org/10.1007/s12576-019-00678-5
I’m Dizzy and Sometimes Off Balance: Could I have a Vestibular Disorder?
 Feeling dizzy or off balance can be unsettling and frustrating. You might wonder what's causing these sensations and how to get back to feeling steady. One possible cause could be a vestibular disorder. As a chiropractic neurologist, I want to help you understand what vestibular disorders are and how we can address them together.
Feeling dizzy or off balance can be unsettling and frustrating. You might wonder what's causing these sensations and how to get back to feeling steady. One possible cause could be a vestibular disorder. As a chiropractic neurologist, I want to help you understand what vestibular disorders are and how we can address them together.
Understanding Vestibular Disorders
Your vestibular system, located in your inner ear, plays a crucial role in maintaining your balance and spatial orientation. When something goes wrong with this system, you might experience dizziness, vertigo (a spinning sensation), imbalance, and other related symptoms. These issues can stem from various causes, including infections, injuries, or even aging.
Common Symptoms of Vestibular Disorders
- Dizziness: A feeling of lightheadedness or unsteadiness.
- Vertigo: The sensation that you or your surroundings are spinning.
- Balance Issues: Difficulty standing or walking without falling.
- Nausea: Feeling sick to your stomach, sometimes accompanied by vomiting.
- Visual Disturbances: Blurry vision or difficulty focusing.
If you're experiencing any of these symptoms, it's essential to seek help from a specialist who understands vestibular disorders and can use vertigo treatments to help.
The Role of a Vestibular Specialist
A vestibular specialist can accurately diagnose and treat vestibular disorders. These professionals have specialized training to pinpoint the exact cause of your symptoms and develop an effective treatment plan. As a chiropractic neurologist, I combine my expertise in both chiropractic care and neurology to offer a unique approach to managing vestibular disorders.
Why Choose a Chiropractic Neurologist?
Chiropractic neurologists are trained to understand the complex relationship between your nervous system and overall health. We use non-invasive techniques to address the root cause of your symptoms. Here are some ways that a chiropractic neurologist can help:
- Comprehensive Evaluation: I will conduct a thorough assessment of your symptoms, medical history, and any previous treatments you've tried. This helps us understand the underlying issues affecting your vestibular system.
- Personalized Treatment Plan: Based on your evaluation, I will create a customized treatment plan tailored to your specific needs. This plan may include exercises, lifestyle changes, and chiropractic adjustments to improve your balance and reduce dizziness.
- Non-Invasive Techniques: My approach focuses on gentle, non-invasive techniques that promote healing without the need for medication or surgery. This can include vestibular rehabilitation exercises, balance training, and specific chiropractic adjustments.
- Ongoing Support: Managing a vestibular disorder is an ongoing process. I provide continuous support and adjustments to your treatment plan as needed, ensuring you make steady progress and regain your balance.
How Chiropractic Care Can Help
Chiropractic care is a holistic approach that focuses on the body's ability to heal itself. By ensuring your nervous system is functioning optimally, chiropractic care can help alleviate symptoms of vestibular disorders. Here are some ways it can help:
Improving Balance and Coordination
Vestibular rehabilitation exercises are a cornerstone of treating vestibular disorders. These exercises aim to retrain your brain to process balance signals more effectively. As a chiropractic neurologist, I can guide you through specific exercises designed to improve your balance and coordination.
Reducing Dizziness and Vertigo
Chiropractic adjustments can help realign your spine and improve the function of your nervous system. This can reduce the frequency and intensity of dizziness and vertigo episodes. By addressing any misalignments in your spine, we can ensure that your nervous system communicates effectively with your vestibular system.
Enhancing Overall Well-being
A well-functioning nervous system is crucial for overall health. Chiropractic care not only helps with vestibular disorders but also enhances your overall well-being. By improving your nervous system's function, you may experience better sleep, reduced stress, and increased energy levels.
Diving Deeper into Vestibular Disorders
Now that we have a basic understanding of vestibular disorders and how chiropractic care can help, let’s delve deeper into some specific aspects of these conditions.
Types of Vestibular Disorders
There are several types of vestibular disorders, each with its own set of causes and symptoms. Some of the most common include:
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is one of the most common causes of vertigo. It occurs when tiny calcium particles, known as canaliths, become dislodged and enter the semicircular canals of your inner ear. This can cause brief episodes of vertigo when you move your head in certain ways.
Meniere’s Disease
Meniere’s disease is a chronic condition that affects the inner ear. It can cause vertigo, hearing loss, tinnitus (ringing in the ears), and a feeling of fullness in the ear. The exact cause of Meniere’s disease is unknown, but it is thought to be related to fluid buildup in the inner ear.
Vestibular Neuritis
Vestibular neuritis is an inflammation of the vestibular nerve, which carries balance signals from your inner ear to your brain. This condition often results in severe vertigo, dizziness, and balance issues, but does not affect hearing.
Labyrinthitis
Labyrinthitis is similar to vestibular neuritis but also affects the cochlea, a part of the inner ear responsible for hearing. This can cause both vertigo and hearing loss.
Diagnosing Vestibular Disorders
Diagnosing vestibular disorders requires a comprehensive evaluation, including a detailed medical history and various tests to assess your balance and hearing. As a vestibular doctor, I use several diagnostic tools to pinpoint the exact nature of your disorder:
- Audiometric Testing: To evaluate your hearing function.
- Videonystagmography (VNG): To assess eye movements and balance function.
- Rotary Chair Testing: To test the vestibular system’s response to movement.
- Posturography: To measure how well you can maintain your balance under different conditions.
Personalized Treatment Plans
Once we have a clear diagnosis, we can develop a personalized treatment plan tailored to your specific needs. Treatment plans for vestibular disorders often include a combination of the following approaches:
Vestibular Rehabilitation Therapy (VRT)
VRT involves specific exercises designed to improve your balance and reduce dizziness. These exercises help retrain your brain to process balance signals correctly. VRT can be incredibly effective for conditions like BPPV, vestibular neuritis, and labyrinthitis.
Chiropractic Adjustments
Chiropractic adjustments can help improve the function of your nervous system, which in turn can alleviate symptoms of vestibular disorders. By ensuring that your spine and nervous system are properly aligned, we can enhance your body’s ability to maintain balance and coordination.
Nutritional Counseling
Diet can play a significant role in managing symptoms of vestibular disorders. For instance, reducing salt intake can help manage Meniere’s disease by minimizing fluid retention in the inner ear. As part of your treatment plan, I can provide guidance on dietary changes that may benefit your condition.
Stress Management
Stress can exacerbate symptoms of vestibular disorders. Incorporating stress management techniques such as mindfulness, meditation, and gentle exercise can help reduce symptoms and improve your overall well-being.
Living with a Vestibular Disorder
Living with a vestibular disorder can be challenging, but with the right treatment and support, you can manage your symptoms and improve your quality of life. Here are some tips for coping with vestibular disorders:
Stay Active
Regular physical activity can help improve your balance and overall health. Gentle exercises like walking, yoga, and tai chi can be particularly beneficial.
Maintain a Healthy Diet
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support your overall health and well-being. If you have Meniere’s disease, reducing salt intake can help manage your symptoms.
Stay Hydrated
Dehydration can worsen symptoms of dizziness and imbalance. Make sure to drink plenty of water throughout the day.
Manage Stress
Chronic stress can make vestibular symptoms worse. Incorporate stress management techniques such as deep breathing, meditation, and relaxation exercises into your daily routine.
Seek Support
Living with a vestibular disorder can be isolating, but you don’t have to go through it alone. Seek support from family, friends, or support groups to share your experiences and find encouragement.
Taking the First Step
If you're tired of feeling dizzy and off balance, it's time to take action. As a vestibular specialist in Raleigh, NC, we are here to help you regain your stability and improve your quality of life. With the right approach and support, you can overcome the challenges of a vestibular disorder and feel like yourself again.
To schedule a consultation, visit our website to schedule online or call us today. Let’s work together to find the root cause of your symptoms and create a path to better health.
Severe TBIs vs. Concussions: What You Should Know
Severe TBIs vs. Concussions: What You Should Know
Traumatic brain injuries (TBIs) encompass a broad spectrum of head injuries, ranging from temporary concussions to permanent life-altering events. Understanding the differences between concussions and more severe types of TBIs is crucial when seeking treatment.
Here at Carolina Brain Center, we have years of experience dealing with TBIs, concussions, and other neurological conditions. We know how to recognize their respective signs and symptoms, and that allows us to identify the best possible paths to recovery for our patients.
To help you understand the difference between severe TBIs vs. concussions, we’ve put together the following guidelines. The more educated you are about your own condition, the better equipped you are to make the right choices during your recovery. For more information about TBIs and concussions, visit Carolina Brain Center today.
Severe TBIs vs Concussions: What’s the Difference?
Concussions are considered mild traumatic brain injuries. They often result from a blow, jolt, or sudden movement to the head or body, causing the brain to shake within the skull. While concussions are generally not life-threatening, they can lead to a range of symptoms that affect cognitive, physical, and emotional well-being.
Severe TBIs, on the other hand, involve more extensive damage to the brain and can have life-threatening implications. These injuries typically result from a forceful impact, penetration, or severe shaking of the head, leading to significant disruption of brain function.
Signs and Symptoms
Concussions
- Loss of Consciousness: Zero to 60 seconds.
- Headache: Often the most common symptom after a concussion.
- Dizziness or Vertigo: Feeling lightheaded, off-balance, or experiencing a spinning sensation.
- Nausea or Vomiting: Feeling queasy or actually vomiting post-injury.
- Temporary Confusion or Disorientation: Momentary disorientation, trouble focusing, or memory problems.
- Sensitivity to Light or Noise: Heightened sensitivity to light or sound.
- Fatigue: Feeling unusually tired or having low energy levels.
Severe TBIs
- Loss of Consciousness: Unconsciousness after the injury, ranging from minutes to hours.
- Severe Headache: Intense and persistent headaches following the injury.
- Seizures: Sudden, uncontrolled electrical activity in the brain.
- Slurred Speech or Incoherence: Difficulty speaking or forming coherent sentences.
- Numbness or Weakness: Loss of sensation or motor function in limbs.
- Persistent Confusion or Agitation: Long-lasting disorientation or emotional disturbances.
Recovery Paths

Concussions
- Rest and Observation: Adequate rest, both physical and cognitive, is crucial for concussion recovery.
- Gradual Return to Activities: Slowly reintroducing activities as symptoms improve under medical guidance.
- Monitoring Symptoms: Consistent monitoring of symptoms to ensure they don't worsen during recovery.
- Functional Neurology: Receiving treatment for an experienced functional neurology professional can help exercise your brain and restore it to full health.
Severe TBIs
- Hospitalization and Medical Intervention: Immediate medical attention and intensive care may be necessary.
- Rehabilitation Programs: Specialized therapies involving physical, occupational, and speech therapies to regain lost function. Functional neurology can also help relieve symptoms and enhance the healing process.
- Long-Term Monitoring: Continual monitoring and follow-up care to manage ongoing symptoms and potential complications.
Carolina Brain Center Treats TBIs, Concussions, and More!
Knowing how to identify severe TBIs vs. concussions is essential for accurate diagnosis and appropriate treatment. While concussions often resolve with rest and time, severe TBIs may require extensive medical intervention and rehabilitation. Recognizing the signs, promptly seeking medical attention, and following recommended recovery protocols is critical for optimizing outcomes and ensuring the best possible recovery for individuals affected by these injuries.
If you or someone you love has suffered a traumatic brain injury, Carolina Brain Center can help guide you down the road to recovery. We believe in a holistic and patient-centered approach to care, which is why we tailor our treatment plants to the specific needs and capabilities of each individual patient.
Let’s work together to design the perfect treatment plan for you; contact us today!
What Are Ketones? An Introduction to the Neurological Benefits of Ketone Therapy
Ketones have been gaining more and more attention in recent years, in part due to the popularity of ketogenic diet plans for weight management. However, many people still don’t know much about them. What are ketones? And, besides weight management, what potential health benefits do they offer? Can ketones be used to improve neurological function?
Believe it or not, they can. Ketone therapy, which involves the deliberate elevation of ketone levels in the body, has shown to be extremely beneficial in the field of functional neurology, especially when used in conjunction with hyperbaric oxygen therapy. That’s why Carolina Brain Center is proud to partner with deltaG Ketones to offer our patients ketone therapy services.
A WADA, BSCG, & FDA GRAS-approved ketone supplement, deltaG Ketones were developed by scientists at the University of Oxford and the National Institutes of Health. Below, we’ll delve into how these ketones work and what benefits they offer functional neurology patients. To experience firsthand what deltaG Ketones can do for you, contact Carolina Brain Center today!
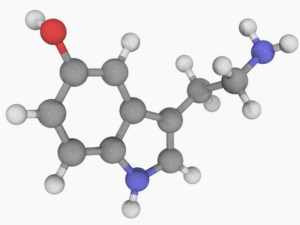
What Are Ketones?
Ketones are molecules produced when the body breaks down fats for energy in the absence of sufficient carbohydrates. They serve as an alternative fuel source for the brain and muscles when glucose availability is limited, such as during fasting, a low-carbohydrate diet (like the ketogenic diet), or prolonged physical exertion.
The three main types of ketones produced in the body are beta-hydroxybutyrate (BHB), acetoacetate, and acetone. Of these, BHB is the most abundant. In fact, BHB can itself be divided into two subtypes: D-BHB (which supplies the body with efficient energy) and L-BHB (which is used less for energy and more to synthesize fatty acids).
High amounts of D-BHB can be found in deltaG Ketones, enabling patients to enjoy the benefits of ketone therapy without necessarily having to change their diet.

Benefits of Ketone Therapy
Ketone therapy involves intentionally elevating blood ketone levels through dietary modifications, supplementation with ketone salts or esters, or fasting regimens. This therapeutic approach has garnered attention for its potential in various health realms, including weight management, cognitive enhancement, epilepsy treatment, and neuroprotection.
By inducing a state of nutritional ketosis, ketone therapy offers several potential benefits:
Enhanced Cognitive Function
One of the most notable benefits of ketones is their capacity to enhance cognitive function. Research indicates that ketones serve as a more efficient and cleaner fuel for the brain compared to glucose, leading to improved mental clarity, focus, and concentration. Moreover, ketones have shown potential in mitigating the cognitive decline associated with aging and certain neurodegenerative conditions, offering hope for individuals seeking to preserve their cognitive abilities.
Neuroprotective Effects
Ketones exhibit neuroprotective properties that can safeguard the brain against various neurological disorders. Studies suggest that ketones possess antioxidant and anti-inflammatory properties, which help reduce oxidative stress and inflammation—two significant contributors to neurodegeneration. Additionally, ketones may enhance the production of brain-derived neurotrophic factor (BDNF), a protein crucial for neuronal survival and growth, further promoting neuroprotection.
Management of Neurological Conditions
Ketone therapy has emerged as a potential adjunctive treatment for various neurological conditions. Conditions such as epilepsy, where traditional treatments might be inadequate, have shown promising responses to ketogenic diets or exogenous ketone supplements. The anticonvulsant effects of ketones have provided relief to many individuals, especially those with drug-resistant epilepsy.
Moreover, research into the therapeutic applications of ketones in neurodegenerative disorders like Alzheimer's disease, Parkinson's disease, and even traumatic brain injury suggests that ketones can help patients manage these conditions by slowing down disease progression and improving symptomatology.
Improved Energy Metabolism and Brain Health
Ketone bodies act as an efficient energy source for the brain, particularly during times of glucose scarcity. This metabolic flexibility not only sustains brain function but also promotes overall brain health. Ketones provide a more stable and consistent energy supply, reducing the fluctuations commonly associated with glucose metabolism. This stability contributes to sustained mental clarity and alertness, which can benefit individuals seeking peak cognitive performance.
Weight Management and Metabolic Health
As noted earlier, ketone therapy has proven effective for weight management and improving metabolic health. Ketogenic diets, which induce ketosis by significantly reducing carbohydrate intake, have been effective in promoting weight loss and improving metabolic markers like blood sugar levels, insulin sensitivity, and cholesterol profiles. These metabolic improvements can benefit brain health, as conditions like insulin resistance and diabetes are linked to an increased risk of cognitive decline.
Learn More About deltaG Ketones at Carolina Brain Center
While the benefits of ketones for functional neurology patients are impressive, we’ve only just begun to scratch the surface. Now that you know how to answer the question “What are ketones,” the next important thing to ask is “What else can ketones do for us?”
As ketone research continues and more neurological benefits are uncovered, there’s one you can be certain about: Carolina Brain Center will be there every step of the way. We strive to provide our patients with the best and most up-to-date neurological health services. That’s why we’ve chosen deltaG Ketones to be our supplier of ketone supplements.
Do you think deltaG Ketones might be for you? Come into Carolina Brain Center today and let us develop a personalized treatment plan just for you!
Natural Migraine Treatment: The Role of Nutrition & Lifestyle Changes in Migraine Management
Migraines are often debilitating and disruptive, and they affect millions of people worldwide. The result? Many people are unsure where to turn for effective, natural migraine treatment.
That’s where Carolina Brain Center comes in. Here at Carolina Brain Center, we believe in a holistic, patient-centered approach that emphasizes treating the whole person, not just the symptoms. When traditional medications aren’t enough, we’ve found that making small but fundamental changes to diet and lifestyle often helps patients reduce migraine frequency, severity, and overall impact on daily life.
In this post, we’ll look at some helpful migraine nutrition and lifestyle tips. By following these recommendations, you’ll be better equipped to manage your migraines in a healthy, non-invasive way. To learn more about holistic approaches to migraine management, schedule an appointment with Carolina Brain Center!
Understanding the Migraine-Diet Connection
Migraine nutrition plays a crucial role in symptom management. Certain foods and beverages are known triggers for migraines in susceptible individuals. Common culprits include:
Potential Trigger Foods
- Tyramine-rich foods: Aged cheeses, processed meats, and certain fermented foods.
- Histamine-containing foods: Wine, aged cheeses, and fermented foods.
- Caffeine: Excessive intake or sudden withdrawal can trigger migraines in some individuals.
- Artificial additives: MSG (monosodium glutamate), nitrates, and aspartame may trigger migraines in sensitive individuals.
- Tannins: Found in red wine, tea, and certain fruits.
Migraine Nutrition Recommendations

Embrace Whole Foods
Prioritize a diet rich in whole, unprocessed foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats. This approach minimizes exposure to potential triggers and provides essential nutrients that support overall health.
Maintain Hydration
Staying well-hydrated is crucial for natural migraine treatment. Dehydration can trigger migraines in some individuals. Aim to drink adequate water throughout the day and limit caffeinated beverages, opting for herbal teas or water instead.
Identify and Eliminate Triggers
Keeping a food diary can help identify personal trigger foods. Eliminating or reducing these triggers from the diet may significantly reduce migraine occurrences.
Lifestyle Changes for Migraine Management

Establish Consistent Sleep Patterns
Quality sleep is vital in migraine management. Irregular sleep patterns or inadequate sleep can trigger migraines. Aim for a regular sleep schedule, ensuring sufficient rest each night.
Stress Management Techniques
Stress is a common trigger for migraines. Adopt stress-reducing practices such as mindfulness meditation, yoga, deep breathing exercises, or engaging in hobbies to alleviate stress levels.
Regular Exercise
Regular physical activity can help reduce the frequency and severity of migraines. Aim for moderate exercise, such as brisk walking, swimming, or cycling, which can also alleviate stress and promote overall well-being.
Natural Supplements and Nutritional Support

Magnesium
Magnesium supplementation has shown promise in reducing migraine frequency and severity in some individuals. Consult a healthcare professional to determine appropriate dosages.
Riboflavin (Vitamin B2)
Studies suggest that riboflavin supplementation may help prevent migraines. Again, however, it's advisable to discuss supplementation with a healthcare provider before starting.
Coenzyme Q10 (CoQ10)
CoQ10 supplementation has demonstrated potential in reducing migraine frequency, although further research is needed to conclusively quantify its efficacy as a natural migraine treatment.
Get Professional Migraine Nutrition Guidance Today!
While nutrition and lifestyle modifications offer significant potential in managing migraines, it's crucial to adopt changes gradually and with personalized guidance. The healthcare professionals at Carolina Brain Center can help you develop a natural migraine treatment plan based on your individual triggers, dietary needs, and overall health status.
That isn’t the only way we can help you with migraine management, of course. We’re proud to offer functional neurology for migraine treatment. We know that every patient is different, with their own specific goals and concerns. That’s why we make sure all our patients have their own personalized treatment plan that is unique to them. We can do the same for you. Call us today to set up an appointment!
Exploring GyroStrim’s Potential in Treating Post-Stroke Symptoms
If you or someone you love has survived a stroke, you know that the effects can linger for a long time. Post-stroke symptoms can present significant challenges, impacting an individual's motor function, balance, and overall quality of life. Rehabilitation is often a slow process, and it’s not always easy. Fortunately, ongoing GyroStim research may be able to help change that.
GyroStim is an innovative therapeutic device that has been gaining attention for its potential in post-stroke rehabilitation. Utilizing rotational movements in a controlled environment, GyroStim offers a unique approach to address and potentially alleviate post-stroke symptoms, aiding in recovery and improving functional outcomes.
Carolina Brain Center is proud to offer GyroStim therapy to those struggling with post-stroke symptoms and other neurological issues. If you’re curious about what GyroStim can do for you, don’t hesitate; reach out to us today!
Understanding Post-Stroke Symptoms
Stroke, a leading cause of disability worldwide, can result in a variety of physical and cognitive impairments. Common post-stroke symptoms include muscle weakness, paralysis, impaired coordination, balance issues, and difficulties with speech or cognitive functions. Rehabilitation plays a crucial role in helping individuals regain lost functions and improve their independence following a stroke.
Potential Benefits of GyroStim for Post-Stroke Rehabilitation
GyroStim is a specialized rotational chair system designed to provide controlled multi-axis movement experiences. Patients sit within the GyroStim capsule-like structure, which moves along various axes and can be adjusted to different speeds and patterns. This controlled rotation creates precise vestibular and proprioceptive stimulation, engaging the brain in adaptive responses to the changing environment.

Vestibular Rehabilitation
The vestibular system, responsible for balance and spatial orientation, often suffers damage during a stroke. GyroStim's rotational movements target and stimulate the vestibular system, aiding in its rehabilitation. The controlled motions within the device can thus help retrain and recalibrate the vestibular system, potentially improving balance and reducing dizziness or vertigo associated with post-stroke symptoms.
Neuroplasticity and Motor Recovery
GyroStim's unique rotational patterns offer sensory input that can induce neuroplastic changes in the brain. By engaging various neural pathways, it can promote neuroplasticity—the brain's ability to reorganize and form new connections. This stimulation facilitates motor learning and recovery, aiding in regaining motor functions affected by the stroke.
Cognitive Rehabilitation
While primarily targeting motor and vestibular functions, GyroStim's complex movements can also contribute to cognitive rehabilitation. The multi-sensory stimulation provided by GyroStim's rotations can help improve cognitive processes, such as attention, spatial awareness, and executive functions, aiding in overall cognitive recovery post-stroke.
Research and Clinical Applications
Studies exploring GyroStim's efficacy in post-stroke rehabilitation are ongoing, showcasing promising preliminary results. Clinical applications of GyroStim in stroke recovery typically involve personalized protocols tailored to individual needs. Therapists can adjust the speed, duration, and direction of rotations to address specific deficits and gradually progress as the patient's abilities improve.
Experience the Benefits of GyroStim at Carolina Brain Center
As GyroStim research progresses and the understanding of GyroStim’s effects on post-stroke symptoms deepens, it holds the potential to revolutionize stroke rehabilitation, providing new avenues for improving functional outcomes and enhancing the quality of life for individuals on their journey toward recovery after a stroke.
Here at Carolina Brain Center, we’re committed to providing our patients with the most innovative and cutting-edge treatment options currently available. GyroStim is just one of the many services we offer. No two patients are ever the same, which is why we always create personalized treatment plans to meet our patient’s unique needs. Schedule an appointment now and let us do the same for you!
Cognitive Benefits of HBOT
One of the most exciting and versatile treatments we offer here at Carolina Brain Center is hyperbaric oxygen therapy (HBOT). This non-invasive treatment involves breathing pure oxygen in a pressurized chamber, resulting in increased oxygen levels in the body's tissues.
Beyond its primary use in treating various medical conditions, one of the many benefits of HBOT is its ability to enhance a patient’s cognitive abilities. HBOT has the potential to positively influence brain function and to help individuals with various neurological conditions and cognitive impairments.
To learn more about HBOT’s benefits for cognitive function, schedule an appointment with Carolina Brain Center today!
Understanding Hyperbaric Oxygen Therapy
HBOT involves exposure to oxygen levels higher than atmospheric pressure while inside a hyperbaric chamber. The increased pressure enables the body to absorb more oxygen, which gets dissolved in the bloodstream and reaches tissues and organs at higher concentrations. This heightened oxygen availability stimulates healing processes, reduces inflammation, and promotes tissue repair.
Cognitive Benefits of HBOT
Enhanced Brain Function
Research suggests that HBOT may enhance cognitive function by improving oxygen delivery to the brain. Increased oxygenation supports neuronal activity, aiding in neurotransmission and promoting neural plasticity—the brain's ability to adapt and form new connections.
Neuroprotective Effects
HBOT's oxygen-rich environment has shown neuroprotective properties, potentially shielding the brain from damage caused by injury, stroke, or neurodegenerative diseases. It may help reduce inflammation, protect against oxidative stress, and promote the survival of brain cells.
Improved Cerebral Blood Flow
HBOT has been associated with enhanced cerebral blood flow, which is vital for optimal brain function. By increasing blood flow to areas affected by injury or reduced circulation, HBOT may support the brain's healing processes and mitigate cognitive impairments.
Applications in Neurological Conditions

Traumatic Brain Injury (TBI)
HBOT has shown promise in aiding recovery from traumatic brain injuries. Studies suggest that it may help reduce cognitive deficits, improve cognitive processing, and enhance functional outcomes for individuals with TBIs.
Stroke
Following a stroke, HBOT's ability to increase oxygen availability to affected brain regions may promote recovery by supporting damaged tissue and potentially restoring lost function.
Discover HBOT’s Benefits at Carolina Brain Center
HBOT’s benefits in terms of cognitive function offer a mere glimpse into its broader applications beyond traditional medical uses. By enhancing oxygen delivery to the brain, HBOT shows promise in supporting brain function, aiding in neurorehabilitation, and potentially benefiting individuals with various neurological conditions.
Carolina Brain Center is committed to offering patients the very best holistic neurological care. That’s why we always stay up-to-date with the latest research and advancements in HBOT, GyroStim, and other innovative forms of non-invasive neurological medicine. Let us help you discover the benefits of HBOT therapy. Contact us today!
Cybersickness: How Screen Time Impacts the Visual-Vestibular System
In an era dominated by digital screens, the phenomenon of cybersickness has emerged as an ongoing concern, affecting individuals who spend significant time engaged with virtual environments. Whether you’re young or old, spending your days hunched over a computer screen at work or swiping right on a smartphone in your bedroom, cybersickness can strike anyone, any time.
Similar to motion sickness, symptoms of cybersickness include nausea, dizziness, headaches, and more. But what causes this condition? More importantly, how can we mitigate the effects of excess screen time in time when so much of our daily lives depend on interacting with screens?
Nothing is more important to us here at Carolina Brain Center than empowering people to maintain their neurological health. In this blog post, we’ll walk you through what cybersickness is, the root causes of it, and what you can do to safeguard your brain from its effects.
If you are concerned about your neurological health, don’t hesitate to contact Carolina Brain Center today. Your well-being is our top priority.
What is Cybersickness?
Cybersickness refers to a collection of symptoms experienced when interacting with digital displays, virtual reality (VR) environments, or video games. Symptoms can range from nausea, dizziness, headaches, eyestrain, disorientation, and fatigue to, in severe cases, vomiting.
These discomforts occur due to visual-vestibular conflict. In short, this is a discrepancy between what the eyes perceive and what the vestibular system (responsible for balance and spatial orientation) senses.

What is Visual-Vestibular Conflict?
The human body comprises the visual system, interpreting information from our eyes, and the vestibular system, located in the inner ear, responsible for balance and spatial orientation. Normally, these systems work in harmony to maintain equilibrium. However, when conflicting signals reach the brain from these systems, it triggers the sensation of motion sickness.
Visual-vestibular conflict occurs when the visual system perceives motion from digital screens (such as scrolling, rapid movements, or perspective changes in video games or virtual reality), while the vestibular system senses a lack of corresponding physical movement. This discordance between visual cues and physical sensations confuses the brain, leading to cybersickness symptoms.
Excessive screen time exacerbates these issues, especially in children whose brains are still developing. With the proliferation of smartphones, computers, gaming consoles, and virtual reality devices, people spend more hours engaged with screens than ever before. Prolonged exposure intensifies the mismatch between visual and vestibular cues, increasing the likelihood of experiencing cybersickness symptoms
Mitigating the Effects of Excess Screen Time
Here are some practical tips to mitigate the effects of excessive screen time and reduce the risk of cybersickness:
- Follow the 20-20-20 rule: Every 20 minutes, take a 20-second break and focus your gaze on something at least 20 feet away. This practice helps alleviate eye strain and reduces the chances of cybersickness.
- Adjust screen settings: Optimize your screen's brightness, contrast, and color temperature to reduce eye strain. Use blue light filters or apps that adjust the screen's color temperature for a more comfortable viewing experience, especially before bedtime.
- Take regular breaks: Incorporate short breaks into screen-intensive activities. Stand up, stretch, or take a brief walk to refresh both your mind and body.
- Maintain proper posture: Sit in an ergonomic position while using screens. Ensure your screen is at eye level, and your chair provides adequate back support to prevent neck and back strain.
- Limit screen time: Establish boundaries and allocate specific periods for screen use. Set aside time for outdoor activities, hobbies, or social interactions that don't involve screens.
- Use distance viewing: When possible, switch to distance viewing by taking breaks outside or looking at distant objects. This practice helps relax the eyes and reduces the strain caused by continuous screen use.
- Stay hydrated and well-rested: Proper hydration and quality sleep play a significant role in reducing the impact of excessive screen time on overall well-being.
Step Away from the Screen and Contact Us Now!
Visual-vestibular conflict is just one of many common neurological issues plaguing people all across the country. Carolina Brain Center was founded to help patients from all walks of life get the treatment they need for a wide range of neurological conditions.
From concussions and traumatic brain injuries to neurodegenerative disorders, our goal is to provide patients with the most effective holistic treatment options available. Whatever your problem, we can help. Don’t wait; get the care you need from the experts who know best. Schedule an appointment with Carolina Brain Center today!
What Causes Migraines? Understanding the Migraine-Brain Connection
Characterized by intense, throbbing headaches often accompanied by sensory disturbances, migraines are complex neurological events that impact millions of individuals worldwide. But what causes migraines exactly? And what can be done to relieve the pain of those who suffer from them?
Carolina Brain Center is committed to a holistic approach to healthcare. This means that our focus is on treating not just your symptoms, but you as a whole person. Doing that requires understanding the neurological causes behind a variety of conditions, including migraines.
What’s more, we believe that by helping you understand what causes migraines, we can empower you to make the best choices for your health, quality of life, and peace of mind. To learn more about what Carolina Brain Center can do for you, don’t hesitate; call us today!
Are Migraines a Neurological Disorder?
Yes, migraines are classified as a neurological disorder due to their specific involvement of the nervous system. They are not (as some people mistakenly believe) merely severe headaches. Instead, they are complex events rooted in abnormal neurological processes. The brain's intricate network of neurons, neurotransmitters, and vascular components contributes to the initiation, progression, and resolution of migraines.
The classification of migraines as a neurological disorder is supported by extensive scientific research that has elucidated the intricate neurological pathways and mechanisms involved in migraine pathophysiology. Advanced imaging techniques like functional magnetic resonance imaging (fMRI) and electroencephalography (EEG) have provided valuable insights into the brain activity alterations during migraine attacks, further cementing their neurological basis.
Migraines' neurological nature is evident not only in the headache phase but also in the premonitory symptoms, aura, and postdrome experienced by many individuals. These phases often involve various neurological manifestations, such as sensory disturbances, visual changes, and alterations in mood and cognition, further emphasizing the condition's neurological underpinnings.
Neurological Pathways Involved in Migraines
Migraines are widely recognized as a neurological disorder due to their intricate involvement of the nervous system. These headaches often stem from abnormal brain activity that affects various areas, including the trigeminal nerve, brainstem, and cortical regions.
Neuro-Physiologic Imbalances
Neurotransmitters, the chemical messengers in the brain, also play a role in migraine pathophysiology. Imbalances in neurotransmitters like serotonin, dopamine, and calcitonin gene-related peptide (CGRP) have been associated with migraines. Serotonin levels, for instance, can impact blood vessel constriction and dilation, potentially influencing migraine onset.
Trigeminal Nerve Sensitization
One significant aspect of migraines involves the trigeminal nerve, a cranial nerve responsible for transmitting sensory information from the face to the brain. During a migraine attack, this nerve becomes sensitized, leading to the release of neuropeptides and inflammatory substances. This process results in the dilation of blood vessels and triggers the characteristic pain associated with migraines.
Cortical Spreading Depression
Another key neurological phenomenon implicated in migraines is cortical spreading depression (CSD). CSD involves a wave of neuronal hyperactivity followed by a temporary suppression of neural activity that propagates across the brain's cortex. This wave is believed to trigger visual disturbances (aura) experienced by some migraine sufferers before the onset of the headache phase.
Carolina Brain Center Offers Holistic Migraine Treatment
It’s important to recognize that the answer to the question “Are migraines a neurological disorder?” is a resounding “yes.” This classification of migraines underscores the need for specialized neurological approaches in their management and treatment. Only by treating migraines as a serious and complex condition can patients truly get the care they need.
Here at Carolina Brain Center, we believe that the best way to combat the effects of chronic migraines is through the creation of personalized, patient-centered treatment plans. We know that no two brains are exactly alike, and that’s why no two treatment plans should be exactly alike.
Let’s work together to build a specialized and (most importantly) effective treatment plan just for you. Schedule an appointment with Carolina Brain Center now!