Our Key Focus Areas
Dr. Dane is ready to help. Dr. Dane brings 20 years of experience to the Triangle and has helped many people achieve a healthier brain and body.
Concussions are also called traumatic brain injuries. They result from blows or other impacts to the head that cause the brain to rattle around inside the skull.The effects of a concussion can be short term or long-lasting.
The vestibular system consists of the areas of the brain and inner ear that help people balance themselves, move their heads, and be aware of spatial relationships.
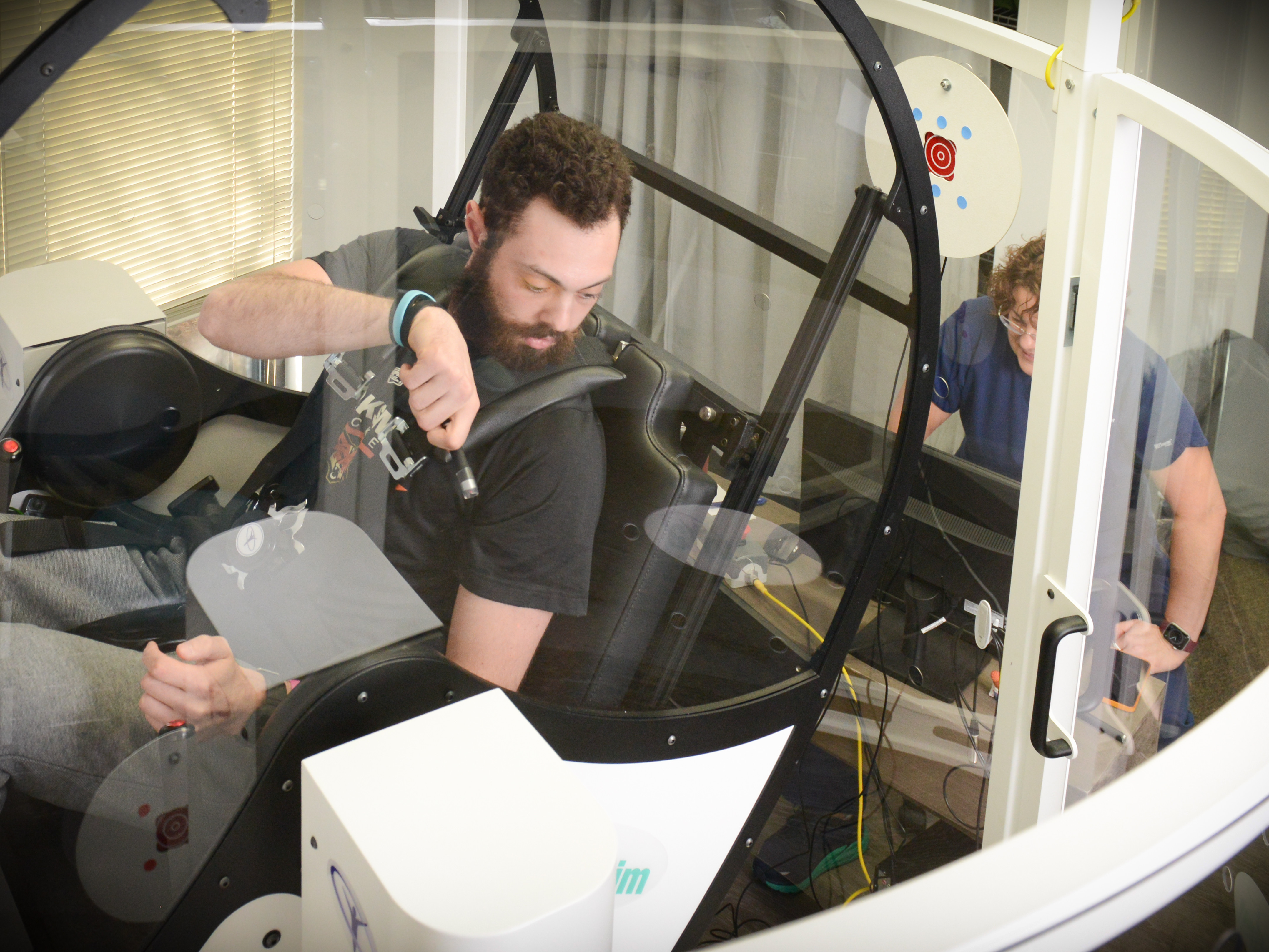
Using a computer-controlled multi-axis rotational chair, GyroStim stimulates the vestibular, visuomotor, and sensorimotor systems of the body to provide powerful and effective treatment for a variety of neurological disorders.
Dr. Dane and her Carolina Brain Center staff are ready to help any and all patients who are just experiencing any of these brain disorders or who have become frustrated with treatments elsewhere and are ready for fresh, effective approaches to functional neurology.
Why Carolina Brain Center?
We understand that far too many people experience these problems and are left without hope. Feeling wholly defeated by a disease or other condition has a devastating effect on moving forward in life and gaining any momentum at all to overcome obstacles. But we have heard many success stories over the years from our patients, from people surviving something they thought they wouldn’t, to parents witnessing their children achieve their potential in school and at home.
Why Carolina Brain Center?
We understand that far too many people experience these problems and are left without hope. Feeling wholly defeated by a disease or other condition has a devastating effect on moving forward in life and gaining any momentum at all to overcome obstacles. But we have heard many success stories over the years from our patients, from people surviving something they thought they wouldn’t, to parents witnessing their children achieve their potential in school and at home.
We provide treatments for people of all ages in Raleigh who are suffering with general neurological symptoms.
Carolina Brain Center provides a wealth of knowledge and treatments associated with neurological conditions.
Patient Satisfaction Is Our #1 Priority!
Our happy patients are the reason physicians in the Triangle trust Carolina Brain Center to analyze, diagnose, and treat a wide range of neurological issues.

“I would like to thank Dr. Dane for the service she provides to many difficult cases we have co-managed. These patients, who have a variety of medical conditions along with visual deficiencies, have been able to improve upon their daily activities through Dr. Dane’s hard work and dedication to her area of specialty. Dr. Dane understands the need to interact with other professionals to provide patients with the best integrative treatment plan in order to achieve the best outcomes.”
Nancy M. Mackowsky, OD, FCOVD
The Mackowsky Visual Learning & Rehabilitation Clinic

“ I am always appreciative of having someone like Dr. Dane to co-manage patients with when they are in need of multiple modes of therapy. This not only positively affects the patient, but also allows us as health care professionals to gain a new perspective that will only further our knowledge and better help patients in the future. At our office, collaboration with other like-minded health care professionals is something we value highly, and I only trust my patients with the best. I know that when they are seeing Dr. Dane, they are getting only the best.”

“I have had the privilege of interacting with Dr. Dane on a professional, academic, and personal level. She has proven to be one of my most intuitive, creative, well-rounded, caring and trustworthy colleagues. All doctors need to consult with their colleagues on occasion. I have access to a network of over 600 colleagues, and Dr. Dane is one of the first colleagues that I reach out to for consultation. Her experience, understanding and clinical proficiency is top-notch. My confidence in her abilities is high enough to refer my family members to her practice, without reservation.”
Matthew Antonucci, DC, DACNB, IMC
www.DrAntonucci.com
Physician Referrals
We love getting patients the care they need. Head to our secure Physician Referral Form and we will get in touch with your patient. Thank you.